This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Rosacea Treatment: 6 Natural Ways to Treat Your Skin
March 27, 2023

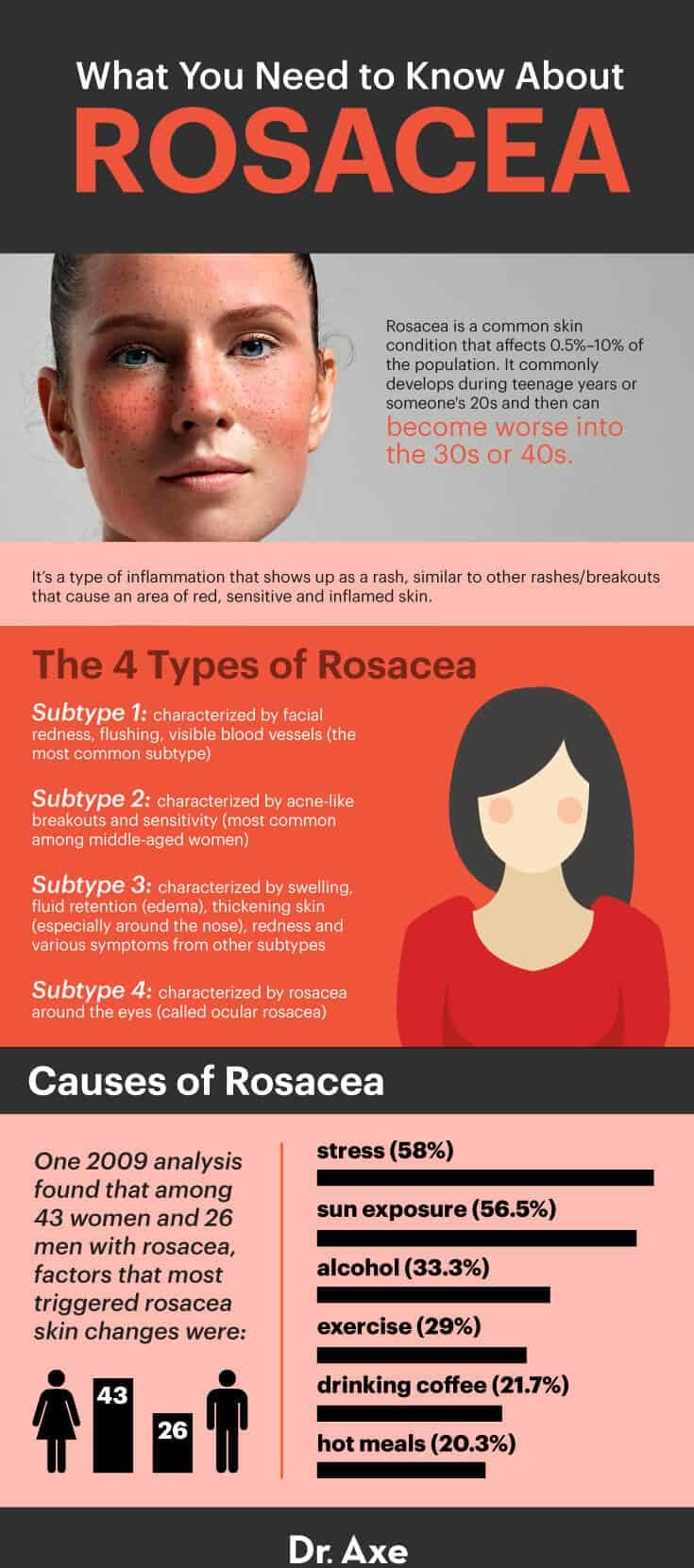
Rosacea is a common skin condition that affects between 0.5 percent to 10 percent of the population, leaving people searching for rosacea treatment options. It commonly develops during teenage years or someone’s 20s and then can become worse into the 30s or 40s. The cause of rosacea is still not entirely understood, though there are many contributing factors.
Meanwhile, the belief in modern medicine is that there’s no real cure for rosacea, and once affected by this condition, someone is likely to experience flare-ups on and off for the rest of his or her life.
While some people might struggle to control their rosacea symptoms from reappearing, many more are able to clear up their skin for good by making certain changes to their lifestyles — and also possibly taking medications at the same time. As you’ll learn, even if you’ve tried several lotions, creams and pills before with no success, there are many holistic steps you can take to help prevent rosacea from causing painful or embarrassing redness, breakouts and irritations.
When it comes to skin flare-ups — whether from rosacea, acne, eczema, hives or other conditions — usually there are some specific triggers that cause skin symptoms to emerge. It isn’t always possible to completely “solve” rosacea, but following the rosacea treatment suggestions below can limit your exposure to triggers that increase inflammation. This helps naturally prevent rashes or at least stops them from becoming worse.
Rosacea Signs and Symptoms
While rosacea affects over 16 million Americans, it appears that most of them aren’t aware they have rosacea. In fact, a National Rosacea Society survey found that prior to diagnosis, 95 percent of rosacea patients knew little to nothing about its signs and symptoms.
Most people equate rosacea with having a red, “flushed” face, but for most people the symptoms go beyond this. Depending on the type of rosacea, people might experience symptoms including:
- Redness in the face, especially toward the center in the cheeks and nose
- “Spider veins,” which are visible broken blood vessels
- Swelling and painful skin
- Sensitive skin that easily reacts to the sun, skin care products, feeling hot or sweating
- Stinging and burning in the skin
- Dry, rough, itchy or scaly skin
- Easily blushing when embarrassed
- Acne-like breakouts and overly oily skin
- Large, visible and inflamed pores
- Raised patches of skin called plaques
- Bumpy texture to the skin
- Parts of the skin that thicken, especially common around the nose (but also can appear on the chin, forehead, cheeks and ears)
- Sensitivity of skin around the eyes, including watery or bloodshot appearance, redness, dryness, stinging, itching, sensitivity to light, blurred vision, cysts, and pain
Rosacea can start out as a small rash or patch of bumps or redness, before spreading and becoming more intense. The condition isn’t contagious, and oftentimes, symptoms can come and go depending on how stressed and run-down you feel, whether or not you’ve been spending lots of time in the sun, and if your diet is triggering any autoimmune reactions.
It doesn’t necessarily get worse over time and for many people can stay relatively constant for many years if necessary steps to resolve symptoms aren’t taken.
Rosacea also takes a psychological toll.
In a survey conducted by the National Rosacea Society, more than 90 percent of rosacea patients reported that their condition lowered their self-confidence and self-esteem, while 41 percent indicated that it caused them to avoid public contact or even cancel social plans. Among rosacea patients with severe symptoms, 88 percent noted that the problem damaged their professional interactions, and over half said they even skipped work because of their skin issues.
Related: Is Dermaplaning Safe? Potential Benefits, Risks, Side Effects & More
Types
Above all, rosacea is a type of inflammation that shows up as a rash, similar to other rashes/breakouts that cause an area of red, sensitive and inflamed skin. Rashes are caused by irritation, allergies, infections, underlying diseases and structural defects of the skin, including blocked pores or malfunctioning oil glands.
Rosacea is similar in nature to other types of skin rashes, including acne, dermatitis, eczema, hives, pityriasis and psoriasis.
There are actually four different subtypes of rosacea, although some people will have symptoms from more than one subtype at a time. The four types of rosacea are:
- Subtype 1 (erythematotelangiectatic rosacea): characterized by facial redness, flushing, visible blood vessels (the most common subtype)
- Subtype 2 (papulopustular rosacea): characterized by acne-like breakouts and sensitivity (most common among middle-aged women), alongside persistent redness, bumps (papules) and/or pimples (pustules) that can be frequent
- Subtype 3 (phymatous rosacea): characterized by swelling, fluid retention (edema), thickening skin (especially around the nose, or rhinophyma), redness and various symptoms from other subtypes
- Subtype 4 (ocular rosacea): characterized by rosacea around the eyes
If these symptoms ring true for you, speak to your dermatologist about whether you might have rosacea, what subtype you likely have — erythematotelangiectatic rosacea, papulopustular rosacea, phymatous rosacea or ocular rosacea — or if you actually have another similar skin condition. Your doctor can diagnose rosacea by examining both your skin and eyes, plus talking about your medical history, genetic factors and lifestyle factors, like your diet and stress levels.
Not every person with rosacea has the same noticeable signs and symptoms present. There are different rosacea treatments that work best depending on the subtype, including if you have the disfiguring rhinophyma, so your doctor will want to look at the specific condition of your skin and eyes in order to know how to best manage your unique case.
In the case that rosacea affects your eyes, you might also need to visit an eye doctor (ophthalmologist), who will know the best way to treat the area surrounding the eyes and how to prevent vision problems from worsening.
Some of the ways that rosacea is commonly treated by dermatologists include:
- Changing your diet to remove any allergies, sensitives or common gut irritants
- Using prescriptions medicines either topically on the skin or taking prescription pills and antibiotics
- Being careful to always wear sunscreen, which helps prevent irritation from UV light, redness and flare-ups
- Receiving skin treatments from your doctor, including dermabrasion, emollients, laser therapy or other forms of light therapy (like electrocautery)
- Taking eye medications or drops when rosacea spreads to the eye lids
Causes
Rosacea is a type of facial skin inflammation. Medical experts still don’t know exactly the series of reactions that causes rosacea to develop, but since it seems to be triggered by heightened inflammation levels and an overactive immune system to some extent, following an anti-inflammatory diet (possibly including an autoimmune-type protocol) helps many people control the severity of their symptoms.
In order to get closer to understanding the causes of rosacea, you must ask what causes inflammation, the underlying cause of rosacea, in the first place? A number of factors likely contribute to the development of rosacea, including:
- problems with blood vessels in the skin
- sun damage/UV radiation that produces vascular changes — researchers at the Boston University School of Medicine concluded that exposure to the ultraviolet (UV) radiation in sunlight spurred the production of vascular endothelial growth factor, a substance that is linked to the development of visible blood vessels (telangiectasia)
- inflammation/abnormal inflammatory reactions within the skin’s connective tissue
- demodex, a microscopic mite that is a normal inhabitant of human facial skin — “evidence appears to be mounting that an overabundance of Demodex may possibly trigger an immune response in people with rosacea, or that the inflammation may be caused by certain bacteria associated with the mites” — in the Journal of the European Academy of Dermatology and Venereology, demodex was found in 15 to 18 times greater numbers in rosacea patients than in healthy subjects
- reactions and side effects to certain medications
- subtypes of rosacea seem to have a genetic factor and might run in families
- people who have light, sensitive skin and light eyes are more likely to have rosacea (including those with northern or western European descent); in fact, some reports show that only around 4 percent of rosacea patients are of African, Latino or Asian descent, yet in European countries like Sweden around 10 percent of all adults have rosacea
- it’s also seen more commonly in women than in men (with some reports showing that three times as many women suffer from rosacea than men)
One 2009 analysis done by the Dermatology Outpatient’s Clinic of Jagiellonian University School of Medicine in Cracow found that among 43 women and 26 men with rosacea, factors that most triggered rosacea skin changes were:
- stress (58 percent)
- sun exposure (56.5 percent)
- alcohol (33.3 percent)
- exercise (29 percent)
- drinking coffee (21.7 percent)
- hot meals (20.3 percent)
In a separate survey of 1,066 rosacea patients conduced by the National Rosacea Society, the most common rosacea triggers included sun exposure (81 percent) and emotional stress (79 percent). Other rosacea triggers included hot weather (75 percent), wind (57 percent), heavy exercise (56 percent), alcohol consumption (52 percent), hot baths (51 percent), cold weather (46 percent), spicy foods (45 percent), humidity (44 percent), indoor heat (41 percent) and certain skin care products (41 percent.) (11)
Natural Rosacea Treatment Options
1. Identify Any Triggers in Your Diet
Since rosacea already makes skin sensitive, many people find that simply addressing the noticeable symptoms — for example, by using harsh chemical creams, prescriptions, light therapy and various lotions — actually winds up making skin symptoms even worse. For some people, these rosacea treatments can lower signs and symptoms, at least temporarily, but they don’t address the root cause of the problem.
Many experts recommend thinking of rosacea as a “whole-body problem” as opposed to just one of the skin. Inflammation stemming from gut-related problems seems to be an especially important issue and root cause of skin disorders.
Your skin is ultimately a reflection of your overall health, after all: how well you digest nutrients, if you have any sensitivities or allergies, how well-balanced your hormone levels are, if you’re getting enough sleep, etc.
Many studies have found an association between skin disorders — including rosacea, acne, dermatitis and psoriasis — and inflammatory gastrointestinal tract disorders. An overactive immune system that causes autoimmune reactions is likely a major contributor to both skin and digestive disorders, including leaky gut syndrome, ulcerative colitis, SIBO symptoms, Crohn’s disease and celiac disease.
People who suffer from these disorders show heightened levels of immunoreactive neurons within their tissues and blood vessels that cause inflammation to progress. This inflammation has the power to change the structure of microbial (bacteria) populations that normally colonize the skin and protect it from damage, redness and rashes.
Since inflammation that shows up on your skin can be a clue that you’re experiencing inflammation within your gut, identifying food triggers is an important first step. The best way to tackle rosacea at its root is likely to approach your diet differently; focusing on anti-inflammatory foods and removing common allergens (at least temporarily to track reactions) can make a huge impact on skin disorders by positively affecting gut health and getting rid of yeast and bad bacteria.
The best foods for treating rosacea include:
- Organic vegetables and fruit — These contain anti-inflammatory compounds, antioxidants to lower oxidative stress and sun damage, and vitamins and minerals that help rebuild healthy skin cells. Leafy greens and orange/yellow fruits and vegetables are especially beneficial since they provide carotenoids that fight damage from sun exposure. Why is choosing organic important? Whenever you can, reduce your exposure to toxins and chemicals that can trigger skin reactions by buying organic.
- Healthy fats — Coconut oil, olive oil, avocado, nuts and seeds (like flaxseeds and chia seeds) can all help reduce systemic inflammation within the gut. These are also important for helping with stress management and proper hormone production. (Plus they help keep you full for longer, so you’re less likely to crave processed foods that can trigger symptoms.)
- High-quality “clean proteins” — The immune system needs enough quality protein to work properly, but some types are most likely to trigger reactions than others. Wild-caught fish like benefit-packed salmon (which provides anti-inflammatory omega-3 fatty acids), cage-free eggs (assuming you don’t have an allergy), grass-fed animal products and legumes are all smart choices.
- Anti-inflammatory foods and herbs — Turmeric, ginger, garlic, onions, cruciferous vegetables (like broccoli, cabbage, collard greens, etc.), carrots, tomatoes and green tea can all help specifically combat skin inflammation, according to studies.
The foods you want to avoid if you have rosacea include:
- Anything that causes allergies — If you have any food allergies or sensitivities that are going unnoticed, this can contribute to leaky gut syndrome, which kicks off autoimmune reactions. Allergens can be different from person to person, so doing an elimination diet can help you narrow down what might be causing symptoms for you personally. Some common allergens include gluten, nuts, shellfish/seafood, dairy or eggs (but allergies can really be caused by any food, such as nightshade vegetables, a type of stone fruit, citrus, FODMAPs, etc.).
- Alcohol and caffeine — Coffee, other caffeinated drinks and alcohol seem to worsen some people’s rosacea symptoms, especially redness and flushing. This differs from person to person, but it’s worth seeing if your symptoms improve when you cut back on both.
- Sugar and processed foods — Sugar is known to worsen inflammation, increase oxidative stress, irritate the gut lining and aggravate skin disorders. Added sugar is found in a high percentage of processed, packaged foods, along with artificial sweeteners/ingredients, preservatives and texture stabilizers that can kick off allergic reactions.
- Conventional dairy products — Many people find that eliminating conventional cow’s dairy (including yogurt, cheese, milk, ice cream, etc.) helps decrease skin-related symptoms.
- Fried foods, trans fats and hydrogenated oils — Refined vegetable oils that are high in omega-6s are pro-inflammatory. These include corn, soybean, safflower, sunflower and canola oils. Fried foods are also hard on the digestive system and can aggravate gut damage.

2. Wear Sunscreen
Anyone with rosacea-type symptoms, or any form of regular redness on the skin, should be careful about regularly using sunscreen on sensitive areas of the skin (especially the face). UV light seems to aggravate rosacea symptoms and can cause inflammation that is linked to its onset.
Studies show that daily skin care regimens, including the use of a sunscreen, offers significant benefits against flare-ups. While getting exposure to the sun is important for vitamin D production within your skin, it’s best to keep your face well-protected.
The sun is considered one of the most strongly aggravating factors of rosacea, according to some studies. Just be careful about the sunscreen you choose, since studies show many sunscreens are toxic and therefore can make symptoms even worse.
3. Use Natural Moisturizers and Cosmetic Products
Clinical assessments observing the skin’s barrier and hydration levels indicate that moisturizing rosacea-prone skin can help restore the skin’s barrier. When patients regularly cleaned and moisturized dry, rough, patchy skin, they found that noticeable symptoms, discomfort and overall sensitivity of skin improved.
It might be tempting to avoid using moisturizer on your skin if you have oily, red or sensitive patches and are also prone to acne breakouts, but a non-chemical and naturally antibacterial skin moisturizer like coconut oil can provide essential acids to the skin without causing breakouts or further irritations.
Wild plants rich in natural oils (including coconuts, aloe and many that are used to make essential oils) are commonly used to treat skin diseases around the world and have been the go-to methods for treating skin problems for centuries. Natural rosacea treatment products tend to be less irritating and are also cheap, safe and easy to obtain compared to prescriptions.
If you do want to try to cover up your rosacea with cosmetics because you feel self-conscious, just be careful since many commercial makeup products can further aggravate rosacea symptoms. Buying gentle and organic cosmetics limits the amount of harsh chemicals you put on your sensitive skin. You can always ask your dermatologist for help choosing gentle cosmetics, too.
4. Manage Stress Levels
Aside from all of the physical symptoms that rosacea can cause, many people also feel mentally and emotionally challenged by this skin condition. A high percentage of rosacea sufferers report feeling less confident due to their appearance.
Ongoing facial blotchiness, bumps and redness can be really hard to handle emotionally (similarly to suffering from acne), but unfortunately stressing over the condition is only likely to make it worse.
Similarly to acne breakouts, stress is known to be a common trigger of rosacea that can bring on flare-ups. Try your best to control stress in your life for two reasons: first because stress makes autoimmune reactions and inflammation even worse, and secondly because you’re likely already under enough added stress when dealing with a rosacea flare-up.
Remember that you can’t always completely avoid symptoms appearing and shouldn’t feel guilty if flare-ups still occur.
At the same time, you’re also not totally helpless and likely have a lot of control over how severe your symptoms get, so try to focus on feeling empowered instead of embarrassed and find natural stress relievers in your life.
Educate yourself about the disorder, learn more about rosacea treatments and be open-minded to trying new approaches in order to help you feel more in control. Use stress-reducing techniques like exercise, meditation, healing prayer and journaling to try to soothe yourself as much as possible.
Keep in mind that despite what some people might assume, rosacea has nothing to do with poor hygiene and is caused by internal factors, so being open and honest about your condition can help you feel better and gain support.
5. Talk to Your Doctor About Medication Options
Many people turn to rosacea treatments including prescription creams, lotions and gels if natural remedies won’t work to manage their symptoms well enough. Recently, the medical community has gained some valuable insights into the pathophysiology of rosacea and has been able to develop several effective rosacea treatments for controlling symptoms.
However, even though they can be helpful, it’s important to realize that these drugs don’t “cure” rosacea and are only used to control symptoms. Rosacea is an inflammatory condition first and foremost, but it isn’t caused by certain strains or bacteria or any virus, so while antibiotics are the most popular treatments prescribed, they really work to help lower the severity of swelling, bumps and inflammation.
Rosacea treatments for the skin usually contain the active ingredient called azelaic acid or the antibiotic metronidazole. Tetracyclines and metronidazole antibiotics (including brand names MetroGel, Metro-Cream, Galderma) have been the go-to medications for years along with azlaic creams, including Azelex, Allergan, Clindamycin, erythromycin and sulfacetamide — sulfurs are also sometimes prescribed.
However, new therapeutic options are now emerging, including vitamin D receptor antagonists.
The active form of vitamin D (1,25-Dihydroxyvitamin D3) is a natural regulator of the antimicrobial peptide in our skin called cathelicidin. While we still have a lot more to learn about the role of cathelicidin in skin disorders, we know that abnormal levels are related to wound healing and skin diseases including psoriasis, rosacea and atopic dermatitis.
In the case of rosacea, some initial research shows that patients might have elevated levels of cathelicidine in their skin, so antagonist medications that block the production of cathelicidine might help lower symptoms and reactivity. In the future, we might see the manipulation of cathelcidines as an effective form of dermatologic interventions, including those for rosacea.
Side Effects of Rosacea Medications:
If you do decide to use prescription rosacea treatments or antibiotics, it’s usually best to try a topical one used on the skin, as opposed to antibiotics capsules taken internally that can affect gut health in negative ways. Antibiotics work by reducing bacteria that contribute to the problem.
However, they not only kill “bad bacteria” in your body, but they also kill “good bacteria” living in the digestive tract that are needed for proper digestion, nutrient absorption, immune defenses and more.
Because skin damage from rosacea can be progressive, some dermatologists prefer that medications be continued with an antibiotic for more than a year. However, this poses risks considering antibiotics have dangers when used often and long term.
Ongoing use increases the likelihood of antibiotic resistance forming, which means the medications can stop working. Pigmentary deposition is another problem, which results when the skin turns abnormal pigments (usually very light) permanently.
6. Try Supplements and Essential Oils that Can Help Rosacea
Many supplements and essential oils can help fight inflammation. Herbal remedies offer a safe and effective way to treat different kinds of skin diseases, even for sensitive skin, which is why they’ve been used in places like India, Asia and Australia for thousands of years.
Even today, more than 80 percent of people in India depend on traditional health care treatments and use various plant-based products for treating skin-related problems!
Many natural plant extracts, spices and herbs do more than just lower red, inflamed breakouts. They can also be effective for fighting bacterial growth, yeast, fungus, signs of aging, wrinkles, stretch marks and hyperpigmentation.
They seem to help speed up circulation and, therefore, wound healing by improving blood flow to the effected area, reducing the presence of bacteria that can aggravate skin and preventing cell death of healthy cells.
Some of the best essential oils and supplement rosacea treatments for reducing skin inflammation include:
- Turmeric
- Ginger
- Aloe vera gel (used topically on the skin)
- Raw honey (used topically on the skin)
- Essential oils: Tea tree, lavender, eucalyptus, geranium, chamomile, rose, rosemary and thyme essential oils have all been found to fight skin inflammation and help treat sensitive skin. To treat the area, simply rub three drops of oil on three times daily mixed with 1/2 teaspoon of coconut oil. Always combine these with a carrier oil (including coconut or jojoba oil), and apply to the affected area no more than twice daily. Perform a skin patch test first, and then start gradually to test results, making sure you don’t experience an allergic reaction.
Final Thoughts
Lastly, I consider it very important to join supportive organizations. The National Rosacea Society and National Institute of Arthritis and Musculoskeletal and Skin Diseases (NAIMS) can both be helpful in helping you understand the disease and be aware of the latest research as well as rosacea treatments.