This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Food Allergy Symptoms + 6 Ways to Reduce Them
July 3, 2023

Food allergies are immune-based diseases that have become a serious health concern in the United States, with an estimated 32 million Americans dealing with food allergy symptoms according to the food allergy research organization FARE.
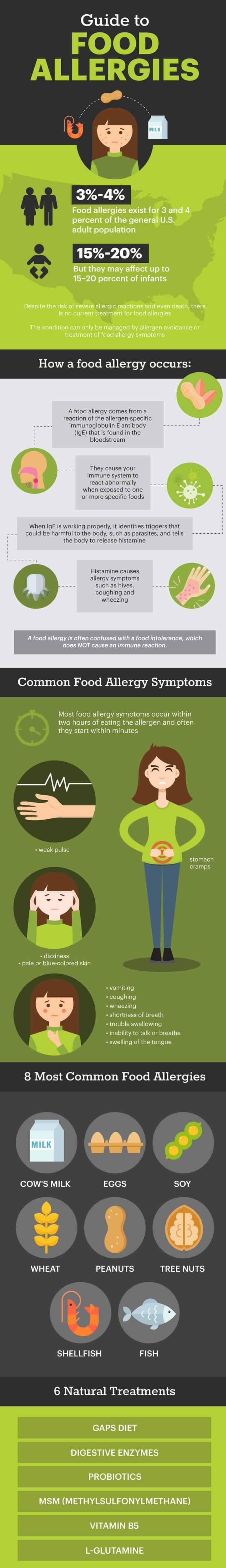
Despite the risk of severe allergic reactions and even death, there is no current cure for food allergies. The condition can only be managed by allergen avoidance or treatment of food allergy symptoms.
Fortunately, there are natural allergy fighters that can help boost the immune system and enhance the gut microbiota, which helps reduce the development of food allergies and food allergy symptoms.
What Are Food Allergies?
Food allergies consist of immune system responses to disagreeable foods. The body senses that a protein in a particular food may be harmful and triggers an immune system response, producing histamine to protect itself. The body “remembers” this, and when this food enters the body again, the histamine response is more easily triggered.
The diagnosis of food allergies may be problematic because nonallergic food reactions, such as food intolerances, are frequently confused with food allergy symptoms. Intolerance derived from an immunological mechanism is referred to as a food allergy, and the non-immunological form is called a food intolerance.
Food allergies and intolerances are often linked, but there’s a clear difference between the two conditions.
A food allergy comes from a reaction of the allergen-specific immunoglobulin E antibody that is found in the bloodstream. Non-IgE-mediated food allergies are also possible. This happens when someone is exposed to a food that causes signs and symptoms of an allergy, such as allergic contact dermatitis.
A food intolerance is an adverse reaction to foods or food components but not due to immunologic mechanisms.
For example, a person may have an immunologic response to cow’s milk because of the milk’s protein, or that individual may be intolerant to milk due to an inability to digest the sugar lactose. The inability to digest lactose leads to excess fluid production in the gastrointestinal tract, resulting in abdominal pain and diarrhea. This condition is termed lactose intolerance because lactose in not an allergen, as the response is not immune-based.
Food intolerances are nonspecific, and the symptoms often resemble common medically unexplained complaints, such as digestive issues.
IgE-medicated food allergies are the most common and dangerous of adverse food reactions. They cause your immune system to react abnormally when exposed to one or more specific foods. Immediate reactions to IgE-mediated food allergies are caused by an allergen-specific immunoglobulin E antibody that floats around in the bloodstream.
When IgE is working properly, it identifies triggers that could be harmful to the body, such as parasites, and tells the body to release histamine. Histamine causes allergy symptoms, such as hives, coughing and wheezing.
Sometimes IgE reacts to normal proteins that are found in foods — and when the protein is absorbed during digestion and enters the bloodstream, the entire body reacts as if the protein is a threat. This is why food allergy symptoms are noticeable in the skin, respiratory system, digestive system and circulatory system.
According to a 2014 comprehensive review published in Clinical Reviews in Allergy and Immunology, the prevalence of food allergies in infancy is increasing and may affect up to 15 percent to 20 percent of infants. Researchers from Mount Sinai School of Medicine suggest that food allergies affect as many as 6 percent of young children and 3 percent to 4 percent of adults.
Updated reports from the Centers for Disease Control and Prevention estimate that 6.2 percent of adults in the U.S. have food allergies, while 5.8 percent of children do.
Researchers suggest that this increase in the prevalence of food allergies may be due to a change in the composition, richness and balance of the microbiota that colonize the human gut during early infancy. The human microbiome plays a vital role in early-life immune development and function. Since IgE-mediated food allergies are associated with immune dysregulation and impaired gut integrity, there is substantial interest in the potential link between gut microbiota and food allergies.
Common Food Allergies
Although any food can provoke a reaction, relatively few foods are responsible for a vast majority of significant food-induced allergic reactions. Here are some of the most common food allergies.
1. Cow’s Milk
Cow’s milk protein allergy affects 2 percent to 7.5 percent of children. Persistence in adulthood since tolerance develops in more than 99 percent of children by age 6.
Numerous milk proteins have been implicated in allergic responses, and most of these have been shown to contain multiple allergenic epitopes (targets that an individual target binds to). IgE-mediated reactions to cow’s milk are common in infancy and non-IgE-mediated reactions are common in adults.
A 2005 study published in the Journal of the American College of Nutrition suggests that the prevalence of self-diagnosed cow’s milk allergy is 10fold higher than the clinically proven incidence, suggesting that a sizable population is unnecessarily restricting dairy products (for allergy purposes).
2. Eggs
After cow’s milk, hen egg allergy is the second most common food allergy in infants and young children. A 2012 meta-analysis of the prevalence of food allergies estimated that egg allergy affects 0.5 percent to 2.5 percent of young children.
Allergy to eggs usually presents itself in the second half of the first year of life, with a median age of presentation of 10 months. Most reactions occur upon a child’s first known exposure to egg, with eczema the most common symptom.
Five major allergenic proteins from the egg of the domestic chicken have been identified, the most dominant being ovalbumin.
3. Soy
Soy allergy affects approximately 0.4 percent of children. According to a 2010 study conducted at John Hopkins University School of Medicine, 50 percent of children with a soy allergy outgrew the allergy by 7 years old.
Prevalence of sensitization after the use of soy-based formulas is around 8.8 percent. Soy formula is commonly used for infants who are allergic to cow’s milk, and research suggests that soy allergy occurs in only a small minority of young children with IgE-associated cow’s milk allergy.
4. Wheat
Gluten-related disorders, including wheat allergy, celiac disease and non-celiac gluten sensitivity, have an estimated global prevalence close to 5 percent. These disorders share similar symptoms, making it difficult to make a clear diagnosis.
A wheat allergy represents a type of adverse immunologic reaction to proteins contained in wheat and related grains. IgE antibodies mediate the inflammatory response to several allergenic proteins found in wheat. Wheat allergy affects the skin, gastrointestinal tract and respiratory tract.
Wheat allergy shows greater prevalence in children who commonly outgrow the allergy by school age.
5. Peanuts
Peanut allergy tends to present itself early in life, and affected individuals generally do not outgrow it. In highly sensitized people, just trace quantities of peanuts can induce an allergic reaction. Research suggests that early exposure to peanuts may reduce the risk of developing a peanut allergy.
According to a 2010 study, peanut allergy affects approximately 1 percent of children and 0.6 percent of adults in the U.S. Peanuts are inexpensive and frequently eaten in unmodified form and as components of many different prepared foods. They cause the largest number of cases of severe anaphylaxis and death in the U.S.
6. Tree Nuts
The prevalence of tree nut allergies continues to increase worldwide, affecting about 1 percent of the general population. These allergies begin most often during childhood, but they can occur at any age.
Only about 10 percent of people outgrow tree nut allergies, and frequent lifetime reactions caused by accidental ingestion are a serious problem.
Nuts that are most commonly responsible for allergic reactions include hazelnuts, walnuts, cashews and almonds. Those that are less frequently associated with allergies include pecans, chestnuts, Brazil nuts, pine nuts, macadamia nuts, pistachio, coconut, Nangai nuts and acorns.
A 2015 systematic review found that walnut and cashew allergies were the most prevalent types of tree nut allergy in the U.S.
7. Fish
According to a study published in Clinical Reviews of Allergy and Immunology, adverse reactions to fish are not only mediated by the immune system causing allergies, but are often caused by various toxins and parasites, including ciguatera and anisakis. (See the list of fish you should never eat.) Allergic reactions to fish can be serious and life-threatening, and children usually don’t outgrow this type of food allergy.
A reaction is not restricted to the ingestion of fish, as it can also be caused by handling fish and intaking the cooking vapors. Prevalence rates of self-reported fish allergy range from 0.2 percent to 2.29 percent in the general population but can reach up to 8 percent among fish processing workers. (16)
8. Shellfish
Allergic reactions to shellfish, which comprises the groups of crustaceans (such as crabs, lobsters, crayfish, shrimp, krill, woodlice and barnacles) and molluscs (such as squid, octopus and cuttlefish), can cause clinical symptoms ranging from mild urticaria (hives) and oral allergy syndrome to life-threatening anaphylactic reactions.
Shellfish allergy is known to be common and persistent in adults, and it can cause anaphylaxis in both children and adults. The prevalence of shellfish allergy is anywhere from 0.5 percent to 5 percent. Most shellfish-allergic children have sensitivity to dust mite and cockroach allergens as well.
A phenomenon called cross-reactivity may occur when an antibody reacts not only with the original allergen, but also with a similar allergen. Cross-reactivity occurs when a food allergen shares structural or sequence similarity with a different food allergen, which may then trigger an adverse reaction similar to that triggered by the original food allergen.
This is common among different shellfish and different tree nuts.
Related: Nanotechnology in Food Science: What You Need to Know
Food Allergy Symptoms
Food allergy symptoms can range from mild to severe and, in rare cases, can lead to anaphylaxis, a severe and potentially life-threatening allergic reaction. Anaphylaxis can impair breathing, cause a dramatic drop in blood pressure and alter your heart rate. It can come on within only minutes of exposure to the trigger food.
If a food allergy causes anaphylaxis, it can be fatal and it must be treated with an injection of epinephrine (a synthetic version of adrenaline).
Food allergy symptoms may involve the skin, gastrointestinal tract, cardiovascular system and respiratory tract. Some common symptoms include:
- vomiting
- stomach cramps
- coughing
- wheezing
- shortness of breath
- trouble swallowing
- swelling of the tongue
- inability to talk or breathe
- weak pulse
- dizziness
- pale or blue-colored skin
Most food allergy symptoms occur within two hours of eating the allergen, and often they start within minutes.
Exercise-induced food allergy is when the ingestion of a food allergen provokes a reaction during exercise. As you exercise, your body temperature goes up, and if you consumed an allergen right before exercising, you may develop hives, become itchy or even feel light-headed.
The best way to avoid exercise-induced food allergy is to avoid the food allergen completely for at least four to five hours before any exercise.
Food Intolerance Test
A systematic approach to diagnosis includes a careful history, followed by laboratory studies, elimination diets and often food challenges to confirm a diagnosis. It’s important to be evaluated and diagnosed by a health care professional or allergist. Self-diagnosis of food allergies can lead to unnecessary diet restrictions and inadequate nutrition, especially in children.
Recently, an increasing number of commercial tests for food allergies are marketed to consumers and health care practitioners. IgG or food intolerance testing is meant to work as a simple means to identify food sensitivities, food intolerances or food allergies, but researchers believe that this is an unvalidated form of testing.
The test checks a person’s blood for immunoglobulin G (IgG), an antibody created by the body to fight a certain allergenic food. Drawn blood is exposed in vitro to a panel of foods and food components.
The degree of total IgG antibody binding to each food is measured to determine if any of the foods create an immune response. The degree of sensitivity or allergy is then graded by a classification scale.
The issue with these types of food allergy tests is that unlike IgE antibodies, which are responsible for allergies, IgG antibodies are found in both allergic and non-allergic people. IgGs are the normal antibodies made by the body to fight off infections.
Researchers believe that the presence of specific IgG to food is actually a marker of exposure and tolerance to the food, not necessarily a sign of an allergy. Therefore, positive test results for food-specific IgG are to be expected in normal, healthy adults and children. For this reason, the likelihood of false diagnoses is increased, and people are left confused by the information provided by the food intolerance test.
Due to the potential misuse of this type of test, there is controversy surrounding testing for food sensitivity, and many researchers believe that these tests are not appropriate for making a diagnosis of food allergy. IgG tests may be additionally anxiety-provoking for parents who elect to purchase food sensitivity tests for a child and then must decide whether to follow the instructions on the test report.
According to research published in Allergy, Asthma & Clinical Immunology, the greatest potential risk of these types of tests is that a person with a true IgE-mediated food allergy, who is at a significant risk for life-threatening anaphylaxis, may very well not have elevated levels of specific IgG to her particular allergen and may be inappropriately advised to reintroduce this potentially deadly allergen into into the diet.
Instead of depending on self-diagnosis or unproven tests, see an allergist, who will begin by conducting a thorough medical history. An allergist will commonly follow a medical history with a combination of tests that will give him enough information to provide a diagnosis. These tests may include a skin trick test, blood test, oral food challenge and food elimination diet.
How to Reduce Symptoms of Food Allergies
There are currently no therapies available to prevent or fully treat food allergies. The management of food allergies consists of avoiding the ingestion of the responsible allergen and knowing what to do if there’s an unintended ingestion.
The following natural treatments for food allergies will help you to cope with the food allergy symptoms and make them less severe.
1. GAPS Diet
The GAPS diet is a meal plan that is designed to repair the gut wall, boost the immune system, stop toxic overload and prevent toxins from entering the bloodstream. It is commonly used for the treatment of autoimmune diseases.
The diet focuses on removing foods that are difficult to digest and damaging to gut flora and replacing them with nutrient-dense foods to give the intestinal lining a chance to heal and seal.
Under the GAPS diet, you avoid processed foods, grains, processed sugar, starchy carbs and potatoes, artificial chemicals and preservatives, and conventional meat and dairy. Instead of eating these inflammatory foods, you focus on consuming healing foods, like bone broth, non-starchy vegetables, organic wild meats, healthy fats and probiotic-rich foods.
2. Digestive Enzymes
The incomplete digestion of food proteins may be linked to food allergies and can cause gastrointestinal symptoms. Taking digestive enzymes with meals can aid the digestive system in fully breaking down food particles, and it serves as a vital food allergy remedy.
3. Probiotics
Probiotic supplements boost immune function and reduce the risk of developing food allergies.
A 2011 study published in Bioscience of Microbiota, Food and Health evaluated 230 infants with a suspected cow’s milk allergy. The infants were randomly allocated to groups that received a mixture of four probiotic strains or placebo for four weeks.
The results showed that probiotics may enhance both inflammation and immune defense of the gut. The probiotic treatment further stimulated the maturation of the immune system since the infants given probiotics showed increased resistance to respiratory infections and improved vaccine antibody responses.
4. Methylsulfonylmethane (MSM)
Research suggests that MSM supplements may be effective in reducing allergy symptoms. MSM is an organic sulfur-containing compound that is used to improve immune function, lower inflammation and help restore healthy bodily tissue. It can be used to relieve digestive issues and skin conditions that are associated with allergy symptoms.
5. Vitamin B5
Vitamin B5 supports adrenal function and can help with control of food allergy symptoms. It is important in maintaining a healthy digestive tract and boosting immune function.
6. L-glutamine
L-glutamine is the most abundant amino acid in the bloodstream, and it can help repair leaky gut and boost immune health. Research indicates that leaky gut, or intestinal permeability, is likely to cause various pathologies, including allergies. Compounds such as glutamine have the mechanistic potential to inhibit inflammation and oxidative stress.
Final Thoughts
- Food allergies are immune-based diseases that have become a serious health concern in the U.S.
- Food allergy symptoms consist of an immune system response to a disagreeable food. The body senses that a protein in a particular food may be harmful and triggers an immune system response, producing histamine to protect itself.
- The majority of food allergies are caused by cow’s milk, eggs, soy, wheat, peanuts, tree nuts, fish and shellfish.
- To diagnose a food allergy, it is important to see an allergist, who will use a variety of tests and a medical history. Food intolerance or IgG tests are controversial, and researchers suggest that they do not produce an accurate diagnosis.
- The only way to “cure” a food allergy is to avoid the allergen. There are some natural remedies that can help alleviate the food allergy symptoms, including probiotics, digestive enzymes, vitamin B5 and following the GAPS diet.













