This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
How to Stop Binge Eating
May 17, 2023

For many people with binge eating disorder, mindful eating feels very difficult, and thoughts about food, body weight and eating are near-constant: Did I eat too much? Do I need to restrict? When should I eat again? What should I eat next? Why can’t I just stop eating? Why am I so out of control around food?
Research shows that oftentimes people with eating disorders don’t fall neatly into one category/diagnosis and tend to display more than one type of abnormal eating behavior, in addition to symptoms of depression and anxiety. For example, it’s common for people with all types of eating disorders to engage in behaviors like overeating, restricting, purging, over-exercising, or taking laxatives or diet pills from time to time.
Experts believe that even when someone struggles with binge eating disorder (or is an emotional eater/overeater who doesn’t have a diagnosable eating disorder), he or she likely also restricts food intake and diets frequently. In fact, dieting, obsessing about weight, displaying symptoms of orthorexia, viewing certain foods as forbidden and going too long without eating are all behaviors that increase someone’s chance of developing binge eating disorder.
What Is Binge Eating?
Binge eating disorder (BED) is a somewhat common type of eating disorder — affecting middle-aged women more than any other group — that’s different than other well-known eating disorders like anorexia nervosa or bulimia nervosa, although it has some things in common with both.
Information about binge eating disorder has been evolving over the past several decades as researchers learn more about what drives compulsive eating, obesity and abnormal eating behaviors, but for now binge eating disorder is defined by the National Eating Disorder Association as recurrent binge eating without the regular use of compensatory behaviors (like vomiting, excessive exercise or using laxatives).
Many people who have had binge eating disorder describe it as a cycle that feels very out of control: binging (often on unhealthy foods that have been deemed “off-limits” or forbidden), followed by feelings of intense shame and guilt, often followed by self-hatred, intense dieting and restricting, and then more binging. Harboring a strong urge to eat along with night eating are also quite common.
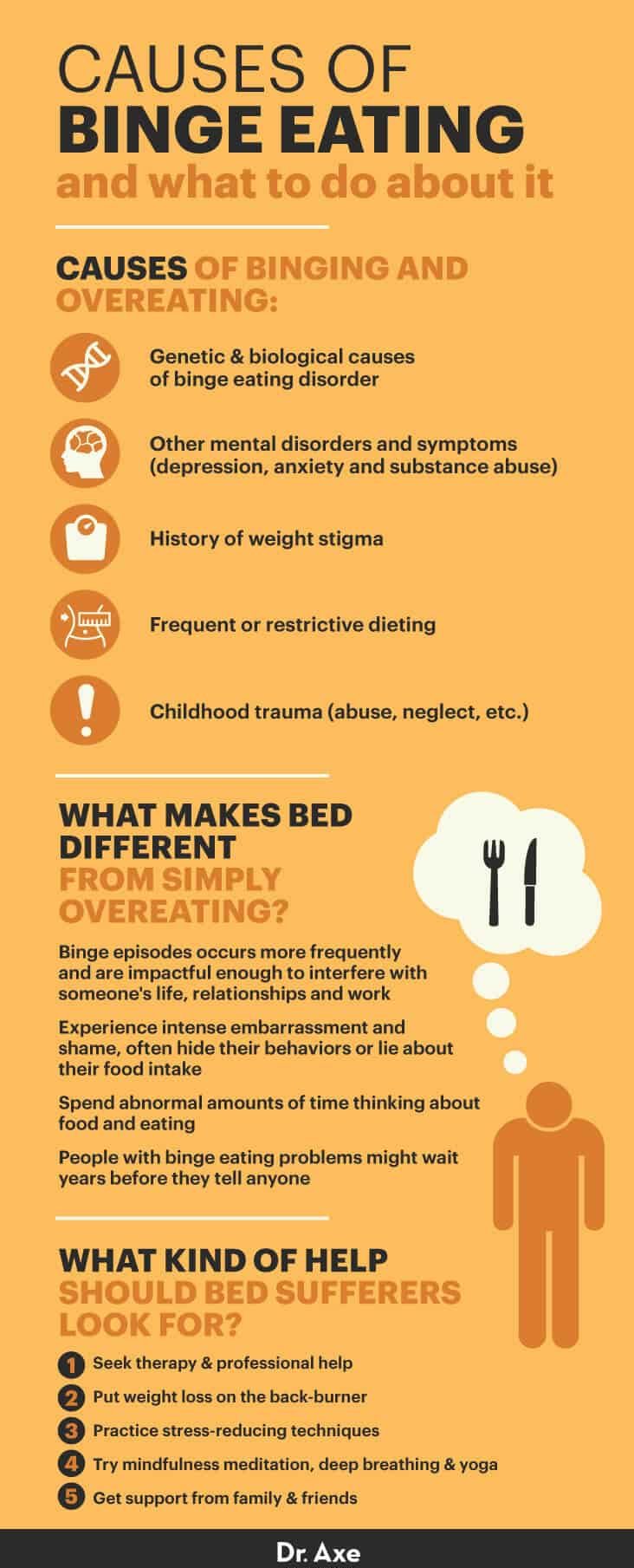
Causes
Like other eating disorders, the cause of binge eating disorder isn’t entirely understood. Researchers state that BED is caused by a combination of genetic, biological, environmental and lifestyle factors. The following play a role in the formation of BED:
- Genetic and biological causes of binge eating disorder: Genes seem to play a role in eating disorders, and it’s clear that BED and other signs of abnormal eating run in facilities. Genes can make it more likely that someone will battle weight gain and find it hard to control overeating throughout that person’s life, although genes alone don’t make someone overweight or have an eating disorder. Experts make it clear that while BED is more likely to affect people who have family histories of eating disorders and obesity, genetics in combination with physical/emotional problems is what leads to destructive thoughts and decisions about food that define BED.
- Other mental disorders and symptoms (depression, anxiety and substance abuse): Studies show that the incidence of depression and anxiety is very high among people with BED. Research suggests there’s likely a cycle taking place, where binge eating contributes to mental problems, including anxiety, and then the mental problems make binge eating harder to manage and break free from. Anxiety, depression, and abusing alcohol and drugs can contribute to negative thought patterns that drive low self-esteem, guilt, shame and hopelessness, which keeps someone trapped in an eating disorder.
- History of weight stigma: Many people with BED feel intense pressure to lose weight and try to meet the “thin ideal” portrayed in society and the media. Experiences of weight stigma, weight-related discrimination, childhood obesity and bullying about weight, and significant history of weight changes are all risk factors for BED.
- Frequent or restrictive dieting: According to research regarding eating disorder statistics, approximately one in five obese adults struggles with binge eating disorder. The majority of obese individuals are fully aware of their problem and attempt to lose weight and control their eating through dieting, which are sometimes very restrictive (such as fasting, fad-dieting or crash-dieting), which can trigger “starvation mode” and intense urges to overeat. For people with BED, following a traditional weight loss program long term seems to be difficult, and many go through cycles of losing and regaining weight over and over again.
- Childhood trauma (abuse, neglect, etc.): It’s a common theme among people with eating disorders, including BED, to have experienced difficult childhoods. Many people with binge eating problems report turning to food for comfort from a young age and having difficulty breaking this habit in adulthood.
Symptoms
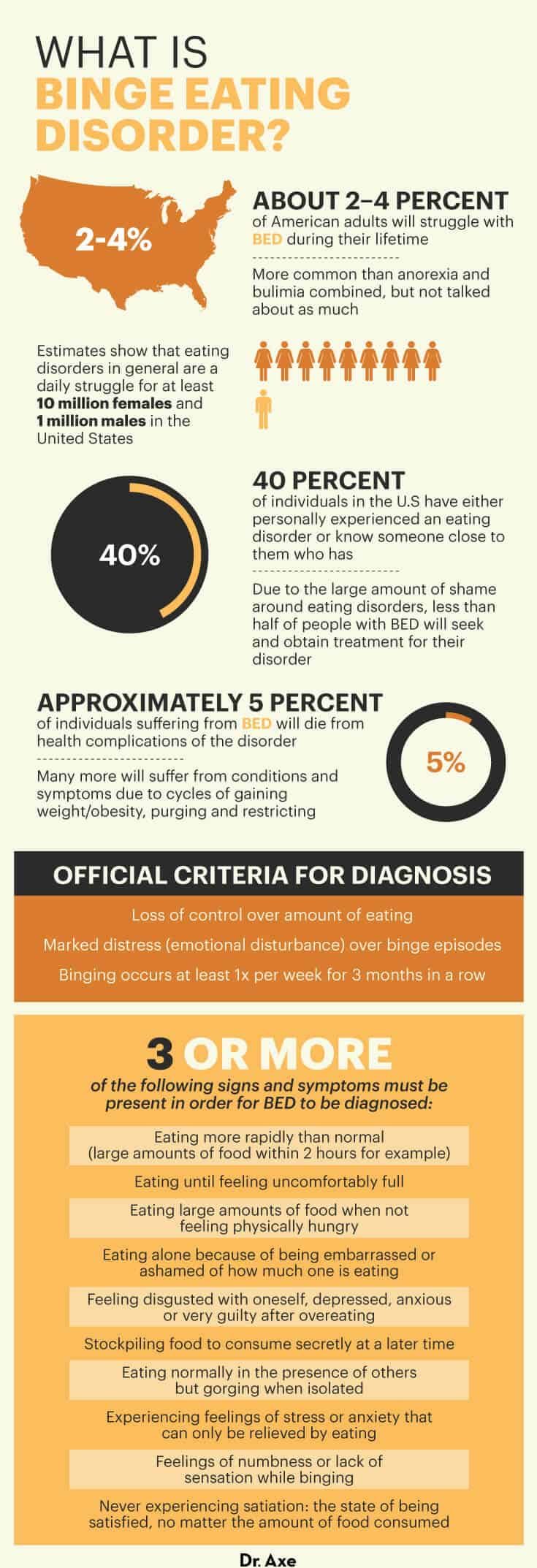
The symptoms and behaviors associated with binge eating are what allow professionals to make a diagnoses and separate BED from other eating disorders, which as mentioned earlier often have some overlap in terms of their symptoms, causes and underlying thought patterns. Currently, the official criteria for diagnosis of binge eating disorder includes:
- Loss of control over amount of eating
- Marked distress (emotional disturbance) over binge episodes
- Binging occurs at least once per week for three months in a row
THREE or more of the following signs and symptoms must be present in order for BED to be diagnosed:
- Eating more rapidly than normal (large amounts of food within two hours, for example, as the urge to eat is very strong)
- Eating until feeling uncomfortably full
- Eating large amounts of food when not feeling physically hungry
- Eating alone because of being embarrassed or ashamed of how much one is eating
- Feeling disgusted with oneself, depressed, anxious or very guilty after overeating
- Stockpiling food to consume secretly at a later time
- Eating normally in the presence of others but gorging when isolated (such as night eating)
- Experiencing feelings of stress or anxiety that can only be relieved by eating
- Feelings of numbness or lack of sensation while binging
- Never experiencing satiation, the state of being satisfied, no matter the amount of food consumed
Aside from the behaviors described above, many people with binge eating disorder experience secondhand physical, emotional and social symptoms related to their overeating, including:
- Higher risk for obesity
- Higher risk for heart disease, diabetes and hypertension
- Increased anxiety, depression and irritability
- Trouble sleeping and insomnia
- Gallbladder disease
- Muscle and joint pains
- Digestive issues, including IBS
How to Stop Binge Eating
1. Seek Therapy and Professional Help
Several forms of professional therapies have been shown to greatly help people struggling with binge eating and start their recovery. These include family-based treatment, adolescent-focused treatment and cognitive behavioral therapy (CBT). CBT is considered by many experts to be the gold-standard approach to treating and managing eating disorders because of how it addresses underlying thought patterns and beliefs that drive compulsive behaviors, shame and anxiety.
CBT (which is the term often used interchangeably with dialectical behavioral therapy) focuses on impulsive interruption and the importance of thoughts in determining behaviors. This type of therapy can help address underlying emotional issues and deeply held beliefs that have nothing to do with food but still drive the desire to overeat, restrict and continue the cycle.
Specifically, there are eating disorder treatment centers that the individual should also consider, if the standard therapies do not seem to work. Serious medical intervention may be required at these treatment centers in order to help reverse this condition.
2. Put Weight Loss on the Back Burner
Because dieting and continuously attempting to lose weight are risks factors for binging, most experts recommend learning to change your entire approach to managing your weight. While it’s important to take good care of yourself, eat healthy foods, and move in the direction of reaching and maintaining a healthy weight, focusing too much on achieving weight loss, obsessing over calorie counting and other restrictive behaviors can actually contribute to anxiety around food. This increases the odds of binging, especially on foods normally viewed as “off-limits.”
A therapist or nutritionist can help you establish an eating plan that seems manageable longterm, meets your calorie and nutrient needs, but still allows room for indulgences and treats. Aiming to eat the “perfect diet,” forbidding or strictly avoiding certain foods, and only focusing on your weight (as opposed to the big picture of your mental and physical health) can actually backfire in the long run. Experts on eating disorders advise that eating for comfort or emotional reasons on occasion is actually normal and not necessarily a bad thing, as long as the food does not become the main source of comfort.
Many therapists and nutrition counselors now use a form of intuitive eating called the “non-diet” method to teach people with BED to recognize and respond to sensations of physical hunger, plus learn to regulate feelings associated with satisfaction, cravings for certain foods and eating for comfort.
3. Reduce Stress
Experts agree that the underlying issues driving eating disorders and binge eating are compulsive behavior and the inability to handle difficult feelings, situations and thoughts. Stress can often trigger the need for people to comfort themselves, and, as we all know, “comfort food” is widely available and often used in this way.
Learning to manage stressful situations or tough emotions without turning to food can feel overwhelming and like a long road if it’s a very ingrained behavior, but it’s essential for recovering from any eating disorder, including BED.
One of the best things you can do for binge eating disorder treatment and boost your odds of recovery long-term is to establish and practice several other ways to soothe yourself and relieve stress during difficult times. Different things work for different people, but studies show that effective stress-reducing techniques include regular exercise, meditation and yoga, listening to music, spending time with other people, reading and writing, being outdoors in nature, and keeping up with fun hobbies.
4. Try Mindfulness Meditation, Deep Breathing and Yoga
Meditation, deep breathing and yoga can all be used as ongoing tools for relaxing, reflecting on tough feelings, boosting creativity, feeling more happiness and gratitude, and even getting better sleep. According to the National Center for Complimentary and Alternative Medicine, mindfulness meditation, healing prayer and yoga learned through guided six- to eight-week programs can reduce binge eating, kickstart eating disorder recovery, improve self-esteem and even improve many aspects of health related to obesity/overeating, including blood pressure, cholesterol, blood sugar and cortisol levels.
Studies have shown that meditation reduces activity in the sympathetic nervous system (responsible for the fight or flight response and anxiety) and increases activity in the parasympathetic nervous system (responsible for emotional control, feelings of calm and clear decision making). One study found that women who took a six-week course of meditation and mindful yoga experienced significantly fewer binge episodes and a reduction in symptoms related to compulsive behavior, stress and depression. “Mindfulness-based eating awareness training” is one type of meditation program designed to address the core issues of BED — controlling responses to varying emotional states, making conscious food choices, developing an awareness of hunger and satiety cues, and cultivating self-acceptance — which has been shown to decrease binge episodes and increase self-control.
Yoga and deep breathing can also improve confidence in someone’s body by increasing appreciation and gratitude for what the body is capable of, regardless of weight. According to the Eating Disorder Hope Foundation, research has demonstrated that practicing yoga and meditation in conjunction with pharmacological and psychological interventions could be a complementary therapy that creates some of the following benefits for people with eating disorders:
-
-
- Increased attentiveness to one’s body functions and feelings (including appetite and fullness signals)
- Improved mood and decreased irritability, plus greater sense of connection and well-being
- Improved body image and self-confidence
- Healing from physical tension and pain (greater muscular strength, cardiovascular function and flexibility)
- Improved ability to focus, sleep, diminish impulsivity and avoid irrational thoughts/behaviors
-
5. Get Support
Getting support from others, especially family and close friends, is crucial to overcoming eating disorders. After all, one of the biggest motivating factors for seeking help and working through recovery is wanting to have closer, more honest and intimate relationships with others. It’s certainly hard to admit when you’re struggling with binge eating, but research shows that being honest and opening up, plus connecting with others going through the same thing, can make all the difference.
You can start gathering support by telling just one person who is close to you about what what you’re going through, becoming educated about BED and joining a support group online. BED support groups can be found through the NEDA (National Eating Disorders Association). It may also help to call an eating disorder helpline.
Binge Eating vs. Compulsive Eating vs. ‘Emotional Eating’
Distinguishing between overeating and binge eating disorder can be difficult even for eating disorder professionals who are well-trained in BED. Binge eating is often thought of as a more severe form of “compulsive” (also called mindless or emotional) eating. All of these terms have been used for decades to describe people’s behaviors who seem to eat large amounts and abnormally. However, BED is considered a distinct entity that is different than overeating, which in the U.S. and many other developed nations is now very common.
Most people who would consider themselves totally “normal eaters” eat for emotional reasons from time to time (not because they’re hungry). This can happen on occasion when dining out with friends, in social situations, on holidays or during vacations. Some people also overeat frequently — such as night eating — even when they’re no longer hungry to deal with feelings like boredom, sadness, being tired or feeling anxious.
But occasionally overeating, eating unhealthy foods or eating for emotional reasons is usually not harmful or destructive in the scheme of things if people are otherwise taking good care of themselves and sticking to clean eating the majority of the time.
What makes BED different from simply overeating is that binge episodes occur more frequently and are impactful enough to interfere with someone’s life, relationships and work. Individuals suffering with binge eating disorder experience intense embarrassment and shame, often hide their behaviors or lie about their food intake, and spend abnormal amounts of time thinking about food and eating.
People with binge eating problems might wait years before they tell anyone — and sadly, the longer it goes on, and the more that people have trouble stopping eating when they’re full and recognizing satiety, the harder the cycle of BED can be to stop.
Facts
- Research regarding the prevalence of binge eating disorder shows that about 2 percent to 4 percent of American adults struggle with BED during their lifetimes (comparatively speaking, around 1 percent struggle with anorexia and 1.5 percent with bulimia). Although BED is more common than anorexia and bulimia combined, historically it hasn’t been talked about as much.
- Binge eating disorder is technically classified as an “other specified feeding and eating disorder” or OSFED, which is “a clinical category of disordered eating that describes individuals suffering from maladaptive thoughts and behaviors related to food, eating and body image, but who do not meet all the diagnostic criteria for another specific diagnosis like anorexia nervosa or bulimia nervosa.”
- Estimates show that eating disorders in general are a daily struggle for at least 10 million females and 1 million males in the U.S., a 40 percent of individuals in the U.S. have either personally experienced an eating disorder or know someone close to them who has.
- Like other eating disorders, binge eating disorder is more likely to happen to an individual who has experienced a psychotic episode by the age of 13.
- Due to the large amount of shame around eating disorders, less than half of people with BED seek and obtain treatment for their disorder (around 43 percent will), which raises various health risks.
- In the DSM-5 (the standard system for classification of mental disorders used by mental health professionals in the U.S.) what’s now called “Binge Eating Disorder” used to be classified under “Eating disorders not otherwise specified” (also called EDNOS, which is now the most common type of eating disorder worldwide).
- Approximately 5 percent of individuals suffering from BED die from health complications of the disorder, and many more suffer from conditions and symptoms due to cycles of gaining weight/obesity, purging and restricting.
Final Thoughts
- Dieting, obsessing about weight, displaying symptoms of orthorexia, viewing certain foods as forbidden and going too long without eating are all behaviors that increase someone’s chance of developing binge eating disorder.
- Researchers believe that BED is caused by a combination of genetic, biological, environmental and lifestyle factors, including genetics and biological attributes, other mental disorders and symptoms, history of weight stigma, frequent or restrictive dieting, and childhood trauma.
- About 2 percent to 4 percent of American adults struggle with BED during their lifetimes (comparatively speaking, around 1 percent struggle with anorexia and 1.5 percent with bulimia).
- Five ways to help treat binge eating disorder include seeking therapy and professional help, putting weight loss on the back burner, reducing stress, trying mindfulness meditation, deep breathing and yoga and getting support from family and friends.











