This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Colon Cancer Symptoms & the Prevention Diet
March 15, 2023

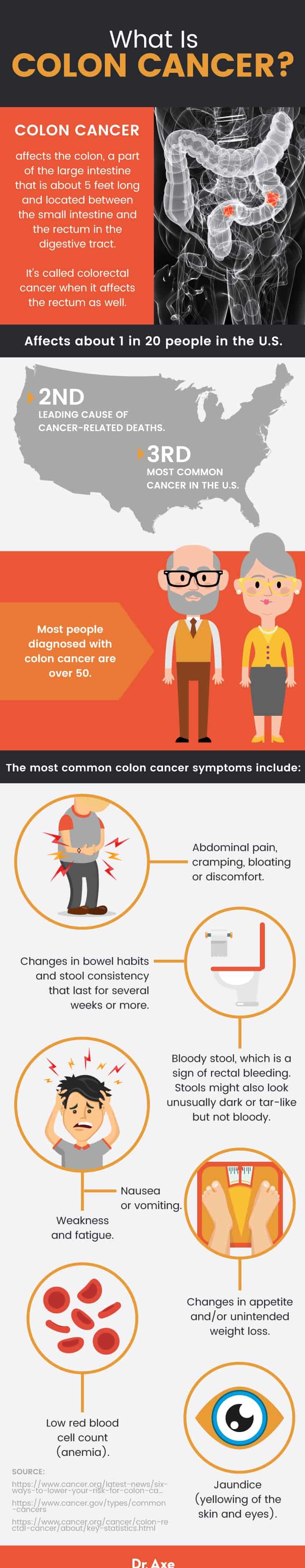
Colon cancer, also called colorectal cancer when it affects the rectum as well, is one of the most prevalent types of cancer. The third most common cancer (after breast and lung cancers), approximately 4.4 percent of men (1 in 23) and 4.1 percent of women (1 in 25) will be diagnosed with colorectal cancer in their lifetime. When the numbers of men and women are combined, it’s the second most common cause of cancer deaths.
Something else that’s alarming? Colorectal cancer rates are even climbing among young people. Only about 5 percent of colon cancer cases are believed to be inherited, which means it’s highly likely that there’s a lot you can do to protect yourself.
Fortunately, in general, the rate of people being diagnosed with colon or rectal cancer each year continues to decline, largely because more people are getting screened and also changing their lifestyle-related risk factors, including learning how to prevent colon cancer.
What are some colon cancer symptoms to be aware of that may indicate a problem? Early signs of colon cancer can include abdominal pain and blood in your stools, although it’s also possible for other disorders to cause these same symptoms. When detected and treated in its early stages, colon cancer can usually be overcome. Research regarding colon cancer survival rates shows that about 90 percent of people with early stages of colon cancer (localized) will live at least five years after being diagnosed. Sadly, once the cancer progresses to stage 3 or 4, about 13 percent to 74 percent will live at least five years.
The earlier that colon cancer is diagnosed, the easier it is to treat. Should you ever be diagnosed with colon cancer, you’ll have the best chances of recovering when you get treatment right away. Below you’ll find much more about the most common colon cancer symptoms, along with ways to lower your risk starting with diet and lifestyle changes.
What Is Colon Cancer?
Colon, or colorectal cancer, is cancer that affects the colon and/or rectum. When cancer is found in both the colon and rectum it is called colorectal cancer, but when it’s found only in the colon it is called colon cancer (or sometimes bowel cancer).
- The colon, which is also called the large intestine, is located between the small intestine and the rectum. It’s about 1 to 1.5 meters long (about 5 feet) and a part of the larger, lower intestinal canal.
- The colon has several parts, including: an appendix, ascending intestine, transverse intestine, and the S-shaped large intestine, which ends at the rectum. The rectum and anal canal make up the last part of the large intestine and are 6 to 8 inches long.
- The colon contains two layers of smooth tissue that are covered by mucosa, which help to absorb nutrients. In the lower large intestine fluids are absorbed and waste is compacted to form stool, which is then stored in the rectum prior to a bowel movement, which eliminates it.
Colon cancer commonly starts developing when small benign clumps of cells that are called adenomatous polyps form in the colon. These can remain non-cancerous or start to form cancerous cells. What are early signs of colon cancer? Abnormal stools (including changes in frequency and appearance) are one of the first indications that a problem may be developing in the colon. Other colon cancer symptoms include changes in appetite, weight loss, nutrient deficiencies and weakness.
Symptoms
How does colon cancer affect a person’s body? Many times colon cancer in its early stages won’t cause any noticeable symptoms. But once it spreads and progresses it can start to change the way that stools are formed, fluids are balanced, nutrients are absorbed and the way that other organs function.
Is there pain associated with colon cancer that might alert you to a problem? Some people with colon cancer experience abdominal pain, although not everyone does. The later the stage of colon cancer, the higher likelihood there is that pain and other colon cancer symptoms will become noticeable and interfere with everyday life.
The most common colon cancer symptoms include:
- Abdominal pain, cramping, bloating or discomfort.
- Changes in bowel habits and stool consistency, such as having diarrhea, constipation, or narrowing and thinning of the stools. Some people experience alternating bouts of constipation and then diarrhea. These symptoms affect almost everyone from time to time, so it’s only really concerning if they last for several weeks or more.
- Bloody stool, which is a sign of rectal bleeding. Stools might also look unusually dark or tar-like but not bloody.
- Weakness and fatigue.
- Nausea or vomiting.
- Changes in appetite and/or unintended weight loss.
- Low red blood cell count (anemia). This can cause symptoms associated with malabsorption of nutrients and anemia, including fatigue, weakness and brain fog.
- Jaundice (yellowing of the skin and eyes).
Risk Factors
Risk factors for colon cancer include:
- Being over the age of 50 (more than 90 percent of people who get colon cancer are over the age of 50).
- Eating a poor diet, especially one high in processed meats, lots of conventional red meat, fried foods, hydrogenated or trans fats, refined grains and other processed foods. Diets that don’t include enough fruits, vegetables and other sources of fiber are linked with a higher risk for colorectal cancer.
- Being obese.
- Being sedentary (not getting enough physical activity).
- High consumption of alcohol, especially among adult men.
- Smoking or using tobacco products.
- A history of other digestive/colon problems, such as pre-cancerous colon polyps, ulcerative colitis, Crohn’s disease, familial adenomatous polyposis (FAP) or hereditary non-polyposis colon cancer (HNPCC).
- Having type 2 diabetes.
- Being African-American. Although it’s not exactly clear why, African-Americans have the highest colon cancer diagnoses and mortality rates out of all the racial groups in the United States. Globally, people who are of Eastern Europe descent seem to have the highest risk.
- Having a family history of cancer.
- Exposure to cancer-causing agents in the environment, including ultraviolet radiation, asbestos, arsenic, radon gas and other chemicals.
Colon Cancer Stages
The CDC recently recommended that adults over the age of 45 have regular colon cancer screenings performed, especially if they are at an increased risk of developing cancer. The age formerly had been 45. The goal of screening for colon cancer is to find the cancer as soon as possible and prevent it from spreading. Screening helps doctors to detect pre-cancerous growths called polyps, which can removed in order to help stop the growth of cancerous tumors.
Colon cancer stages depend on which parts of the colon are affected; if the cancer has spread to the lymph nodes; and if other organs or tissues are impacted (in other words, if the cancer has metastasized). Many times a cancerous tumor that forms in the colon will remain localized (it won’t spread). But in some cases the cancer can spread to other parts of the body including the small intestine, liver, diaphragm or pancreas. When cancerous cells are carried in the bloodstream to other locations in the body, it makes the cancer much harder to treat.
Cancer stages are split into numbers and letters. Numbers range from 0–5, with 0 being the least severe and 5 being the most. Letters A, B and C can be used to indicate sub-stages, with A being less severe and C being more severe. Some doctors also grade cancers, ranging from grade 1 to 4, which indicate how cancer looks when examined under a microscope compared to normal tissue.
Below are the stages of colon cancer and what makes them unique:
- Stage 0 (carcinoma): Diagnosed when cancer has not grown beyond the inner layer (mucosa) of the colon or rectum.
- Stage 1: Diagnosed when cancer has grown through the superficial lining (mucosa) of the colon or rectum. The cancer has not spread beyond the colon wall or rectum (it is localized).
- Stage 2: Cancer has moved through the wall of the colon or rectum. It has not spread to other parts of the body via the bloodstream and has not infiltrated the lymph nodes.
- Stage 3: Cancer has moved to the lymph nodes, a part of the lymphatic system that helps remove waste from the body and prevent illnesses. At this stage the cancer has still not spread to other organs or parts of the body.
- Stage 4: Cancer has spread to other organs and is now difficult to treat.
Conventional Treatments
How do you detect colon cancer? In its early stages colon cancer can be diagnosed in several ways:
- A doctor might find that a patient has noncancerous polyps on a screening test. Polyps usually cause no colon cancer symptoms. When a patient is at an increased risk for having colon cancer, such as due to having risk factors like a family history and being over the age of 50, doctors will usually recommend screenings in order to detect cancer as early as possible.
- A doctor can perform a physical exam by placing pressure on the stomach and intestines, or by inserting one finger into the rectum. Your doctor will check for signs of colon cancer such as inflammation, blood and pain.
- A rectoscopy can be performed to test for the presence of cancerous cells in the colon or rectum. A small tissue sample might be taken in order to perform a biopsy.
- A colonoscopy can also be performed, in which a flexible tube is inserted into the rectum. Tissue samples can also be taken during a colonoscopy.
Treatments for colon cancer will depend on the stage of cancer. Typical treatments can include one or more of the following:
- Surgery, performed to remove polyps, part of the colon lining (a procedure called an endoscopic mucosal resection) or affected lymph nodes. A partial colectomy surgery might also be needed, which involves removing cancerous parts of the colon and then reconnecting healthy portions of the colon and rectum.
- Radiation, which is used to help shrink tumors.
- Chemotherapy, which helps to destroy cancerous cells and prevent spreading.
- Targeted drug therapies or immunotherapy, which are usually used to treat advanced stage cancers and work by targeting specific cells.
How to Prevent Colon Cancer
What are some ways you reduce your risk for colon cancer? Below are strategies for helping to prevent colon cancer, as well as managing colon cancer symptoms such as diarrhea, bloody stools and pain.
1. Increase Antioxidant and Fiber Consumption
Eating foods that promote inflammation and provide little nutritional value has been linked to higher risk for cancer colon. These foods include factory-farm-raised red meat (such as beef, pork or lamb) and processed meats (such as hot dogs, salami and some deli/luncheon meats). It’s even riskier if these meats are cooked at very high temperatures, such as barbecued or roasted.
A November 2017 study published in the Journal of American Medical Association (JAMA) found evidence that increasing fiber intake following colon cancer diagnosis offered patients benefits including improved odds of survival. The eight-year long study included 1,600 adults diagnosed with stage 1–3. All participants completed food-frequency questionnaires for up to eight years following their diagnosis. Researchers found that for every additional 5 grams of dietary fiber that someone ate per day, they experienced a 22 percent decrease in colorectal cancer mortality and a 14 percent decrease in all-cause mortality.
Below are some of the best high-fiber foods to start including in your diet:
- Avocados
- Berries
- Apples and pears
- Coconut flakes
- Figs and dates
- Artichokes
- Okra
- Green peas
- Winter or acorn squash
- Brussels sprouts
- Turnips
- Sweet potatoes
- Beans and legumes, such as black beans, lentils, chickpeas or adzuki beans
- Nuts like almonds or walnuts, flax seeds and chia seeds
- 100 percent whole grains like quinoa, brown rice, buckwheat and rolled oats
There are also other cancer-fighting foods to eat regularly due to how they help lower inflammation and improve nutrient deficiencies. These include:
- Leafy greens like kale and spinach
- Sea vegetables and algae
- Fresh herbs and spices like turmeric, ginger, basil, parsley or oregano
- Raw garlic
- Citrus fruits
- Mushrooms, carrots, beets, tomatoes and bell peppers
- Other cruciferous veggies like broccoli and cauliflower
- Organic, grass-fed or pasture-raised meats
- Wild-caught fish like salmon, mackerel, sardines or herring
- Green tea
- Yerba mate — a study found that yerba mate leaves have both anti-inflammatory and anti-cancer capabilities and that the caffeoylquinic acid derivatives killed colon cancer cells
- Cocoa
- Olive and coconut oil
2. Maintain a Healthy Weight
If you have a history of colon cancer, then staying at a healthy weight may help prevent it from returning. Being overweight or obese has been linked to higher risk for colon and rectal cancer. You can work towards losing weight or maintaining a healthy weight by eating an anti-inflammatory diet, managing stress, getting enough sleep and regularly exercising. Obesity is linked to higher cancer incidence in both men and women, but adult men who are obese seem to be impacted most.
3. Stay Active and Get Enough Exercise
People who are more physically active have better protection against developing colon cancer, as well as overall improvements in health. Some research has found that getting regular exercise may reduce your colon cancer risk by 40 percent to 50 percent! It might also be helpful while in recovery since it improves well-being and can lower stress, depression or anxiety.
Exercise helps to reduce inflammation, improve circulation, support the immune system and can help you control your weight. Getting enough physical activity can also reduce your risk for type 2 diabetes, which is linked to higher colon cancer risk.
4. Limit Alcohol Consumption and Quit Smoking
Studies have found that people who drink high amounts of alcohol and smoke or use tobacco products are more likely to die from colon cancer compared to moderate drinks and non-smokers. Keep your alcohol consumption in check by having no more than two drinks a day if you’re a man, or one drink a day if you’re a woman.
For help quitting smoking, talk to your doctor about useful interventions; speak with a therapist; or start an online program that specializes in smoking cessation.
5. Treat Underlying Health Issues (Such as IBD)
People who have a history of inflammatory bowel disease (IBD), including ulcerative colitis or Crohn’s, may develop dysplasia, which are cells in the lining of the colon that are normal but can become cancerous over time. If you have a history of any health condition that affects your colon, then be sure to get screened regularly.
You can also take steps to prevent IBD flare-ups, although you won’t always be able to control your disorder at all times:
- Eating a therapeutic diet
- Reducing systematic inflammation
- Managing stress
- Getting enough rest and sleep
- Using supplements, such as calcium, vitamin D, probiotics and omega-3 fish oil supplements
- Preventing nutrient deficiencies
- Eliminating certain foods, such as:
- Gluten
- Some FODMAPs
- Caffeine and alcohol
6. Manage Rectal Bleeding
- If it doesn’t worsen colon cancer symptoms or cause pain, eat high-fiber foods that help to relieve constipation, including: cooked green vegetables, beans, squash, prunes, figs, warm bone broths and herbal peppermint tea. Avoid refined flour, pasteurized dairy products, alcohol, caffeine and fried foods.
- If you have hemorrhoids, cleanse yourself only with natural soaps that don’t contain harsh chemicals, alcohol or perfumes. Use plain water to wipe yourself and then dry your bottom afterward. A colon cleanse would not be recommended.
7. Reduce Diarrhea, Constipation & Nausea
If you deal with diarrhea and constipation during your recovery or due to a related illness, here are steps that can help:
- Drink enough water throughout the day. Prevent dehydration when exercising, when you’re sick or when it’s very hot/humid outside.
- Avoid eating very big, high-fat meals. Spacing out meals may make digestion easier.
- Eat enough fiber, but not too much that it worsens symptoms.
- If you have constipation, try having foods and beverages that act as natural laxatives, including: prune juice, psyllium husk, aloe vera, chia and flax seeds, flaxseed oil, cooked leafy greens, probiotic-rich foods like coconut kefir, kombucha, sauerkraut and kimchi, and coconut water. You can also consider taking magnesium supplements or using fiber supplements (although there isn’t evidence this will prevent cancer).
- Incorporate stress-relieving activities into your day, such as yoga, meditation, reading, walking outside, etc.
- If you have nausea, sip on ginger herbal tea or use ginger essential oil. You can also diffuse peppermint or lemon essential oil in your home, try slowly walking outdoors to get fresh air, keep your home cool, and try meditation and acupuncture.
Precautions
If you have any of the colon cancer signs and symptoms mentioned above, rather than panicking it’s best to visit a doctor. Colon cancer symptoms can be similar to those caused by a number of other illnesses, such as hemorrhoids, irritable bowel syndrome, or inflammatory bowel diseases such as ulcerative colitis or Crohn’s disease. In other words, just because you have unusual bowel movements or pain doesn’t mean you have cancer.
That being said, don’t ignore persistent pain or symptoms, especially unusual blood in your stool. Keep up with annual doctor’s appointments and always discuss any risk factors that you may have for cancer with your doctor.








