This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
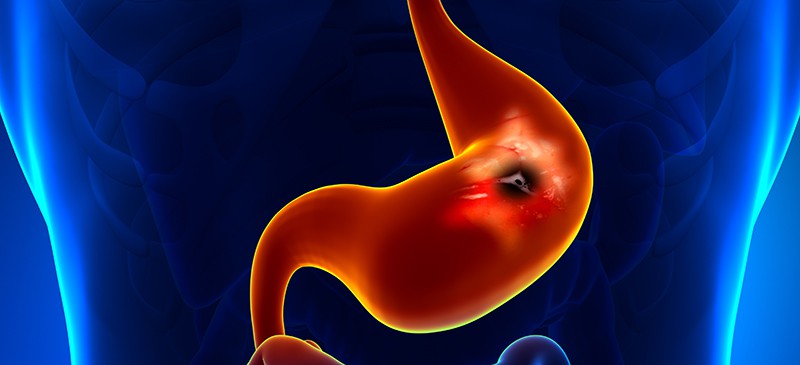
Stomach Ulcer Symptoms You Can’t Ignore and How to Naturally Treat Them
November 13, 2023
Chances are that if you haven’t experienced one yourself, you at least know someone who’s had a stomach ulcer at one point or another. Estimates show that about 500,000 new cases of peptic ulcers are reported each year in the U.S. alone, and at any given time about 5 million people are affected. In addition, one in 10 adults can expect to deal with painful ulcers at one point or another.
For many years, doctors thought that high amounts of stress alone could cause a stomach ulcer to form by increasing production of stomach acid. Then research emerged in the 1980s showing that frequent use of anti-inflammatory drugs, a poor lifestyle and especially a type of bacterial infection caused by the strain Helicobacter pylori (H. pylori) are the real culprits of the majority of ulcers.
Fortunately, according to an article published in the Lancet, prevalence of H. pylori infection and peptic ulcer diseases have become substantially less prevalent than they were two decades ago.
Wondering how to treat a stomach ulcer if you’ve already developed one? Below we’ll cover much more about stomach ulcer treatments — including medications, stress management and dietary changes.
What Is a Stomach Ulcer?
Stomach ulcers (often called peptic ulcers) are painful sores that develop in the lining of your digestive system. They usually form in the stomach but can also sometimes develop in the small intestine (especially a part called the duodenum) or the esophagus.
Here’s the basics of how ulcers work:
Ulcers form when any combination of excess gastric acids, bacteria, drugs or other “toxins” cause damage and small openings to the mucosa, the tissue that lines the stomach, parts of the small intestine and other organs. Mucosa normally protect particles from leaking out.
When someone has an ulcer, hydrochloric acid and pepsin (a type of digestive enzyme that digests proteins) build up and destroy parts of the lining of the gastrointestinal tract. The stomach usually manages acid/pepsin by creating a thick mucus coating that is supposed to act as a buffer between the stomach lining and the acids inside the stomach.
The mucus coating itself usually produces certain chemicals that help repair the stomach lining, keep blood circulating and carry out cellular renewal processes, but some part of this process can become disturbed. When that happens, the lining of the gastrointestinal tract can become exposed, forming small sores (ulcers).
When you eat a meal, food washes the acid in your stomach away temporarily, as it’s used to break down the nutrients in the recently consumed food. Then once your food is digested, the acid once again accumulates in the stomach and can wash against the “raw base” of the ulcer, exposing and opening it up. This causes a burning, painful sensation, sometimes one that’s very strong.
Do stomach ulcers go away? Research shows that by making changes to your diet, plus reducing stress and inflammation, you can help lower your chances of suffering from a stomach ulcer in the first place. If you already have an ulcer, the chances of it healing with lifestyle changes and medications is very good.
Types
Ulcers can develop in various parts of the GI tract, including the esophagus, stomach and duodenum. Contrary to popular belief, research shows that men develop duodenal ulcers (located in the small intestines) more often than any other kind, including stomach ulcers.
On the other hand, the opposite is true for women: They tend to develop more stomach ulcers and fewer ulcers of the duodenal.
Many doctors refer to stomach ulcers simply as peptic ulcers. A few other types of ulcers and names that ulcers sometimes go by include:
- Duodenal ulcers: The duodenum is the proximal portion of the small intestine that is about 10 inches long and plays an important role in the digestion of food, since it holds bile. The bile duct and pancreatic duct both empty into the duodenal, so it can be obstructed or dilated when bile production changes in response to other things going on in the body.
- Esophageal ulcers: This is a peptic ulcer that develops just above your stomach in your esophagus, the tube that carries food from your mouth down to your digestive organs.
- Bleeding ulcers: Unresolved ulcers can start bleeding, which causes other complications. Bleeding ulcers are considered the most dangerous of all. Bleeding internally can also contribute to ulcers when there’s a broken blood vessel in your stomach or small intestine.
- Gastric ulcers: In some people with ulcers, there’s an increase in the amount of hyperacidity of the gastric juices, changing the effects that stomach acid has on the lining of the GI tract. In general, gastric ulcers are another name to describe small openings in the stomach lining that lead to stomach ulcer formation.
Causes and Risk Factors
Ulcers have a unique and interesting history when it comes to their suspected “causes.” For decades, stomach ulcers were considered to be “psychosomatic,” meaning a high-stress lifestyle was to blame.
At the time doctors started identifying high rates of ulcers in hard-working businessmen who smoked a lot of cigarettes and were likely sleep-deprived, and then animal studies further confirmed stress-triggered ulcers. Rats producing high amounts of stomach acid experienced a decrease in stomach ulcer symptoms when researchers fed them antacids, so a connection was then drawn between ulcers, chronic stress and an increase in stomach acid, which changed ulcer treatment approaches forever.
A bacterium called H. pylori was then discovered that seemed to be present in nearly everyone suffering from ulcers. It was also found to run in families and was connected to other digestive disorders, including stomach cancer. In patients given medications/antibiotics to kill H. pylori, ulcers were often resolved at least for a period of time.
However, today it’s more common to treat ulcers using less risky acid-reducing drugs in combination with lifestyle and dietary changes, rather than prescribing antibiotics to kill H. pylori, which can come with complications and lead to antibiotic resistance. Antibiotics used to combat H. pylori can work short term to lower the bacteria but don’t seem to keep it from returning without other interventions.
Ulcers can develop for several reasons. The most common stomach ulcer causes include:
- Infection in the digestive system caused by the bacteria H. pylori. H. pylori is believed to be the cause of most peptic ulcers. Some clinical studies show that H. pylori is found in more than 60 percent of older patients with gastric and duodenal ulcers. Recently it’s become widely accepted that someone’s hygiene and lifestyle can determine whether or not H. pylori causes a problem and any symptoms at all — specifically factors like how much stress and inflammation someone experiences, plus exposure to contaminated food and water. Emerging research, including a 2018 review published in the Journal of Parkinson’s Disease, suggests there’s also a link between H. pylori and Parkinson’s disease (PD). Certain studies have found that people with PD are 1.5- to threefold more likely to be infected with H. pylori than people without PD.
- Long-term use of nonsteroidal, anti-inflammatory medications or over-the-counter drugs (such as NSAID pain relievers like ibuprofen and aspirin, which can lead to ibuprofen overdose).
- Having a run-down immune system caused by high levels of inflammation, a poor diet, high amounts of stress and other poor lifestyle habits.
- Being a woman. In general, women are more likely to have ulcers than men, especially if they’re over the age of 70 and take over-the-counter drugs or medications regularly.
- Smoking cigarettes and excessive alcohol use. Research shows smokers have double the chance of forming ulcers.
- Very rarely from the growth of a tumor (which could be either cancerous or noncancerous) that forms in the stomach, intestines or pancreas (known as Zollinger-Ellison syndrome, which affects only about one in every 1 million people).
- Family history, as ulcers also seem to run in families. Some research shows that people who have relatives with stomach ulcers or duodenal ulcers are two to three times more likely to experience ulcers themselves, and about 50 percent to 60 percent of people with duodenal ulcers report a family history.
- Older age. The peak age for experiencing ulcers is between 55 and 65 years old. As people get older, they tend to have weaker immune systems and higher levels of inflammation, which raises the risk for H. pylori infections that damage the stomach lining and can lead to the formation of “bleeding ulcers.” One longitudinal study published by Oxford Academic found that about 17 percent of older adults admitted to nursing homes had pressure ulcers at the time of admission, and the risk went up to 21 percent by the second year (likely due to the spread of H. pylori bacteria).
Symptoms
Surprisingly, about two-thirds of people found to have peptic ulcers are asymptomatic, according to a 2019 article published in the American Journal of Medicine.
How serious is a stomach ulcer? Ulcer symptoms are not only painful, but can also lead to complications, such as infections, changes in appetite and ongoing nausea/vomiting.
Ulcers can cause a range of symptoms, some that are more mild and go away quickly, but others that linger and cause a good deal of pain. Symptoms of ulcers are usually noticeable and painful, especially when they become severe, such as is the case with a high percentage of duodenal ulcers.
What does stomach ulcer pain feel like? The most common signs of a stomach ulcer include:
- abdominal pains and burning sensations, including bloating (especially after eating and between the belly and breastbone)
- bleeding when vomiting or going to the bathroom
- nausea and vomiting
- darker stools
- loss of appetite and changes in body weight
- trouble sleeping due to pain
- other digestive complaints, like heartburn, acid reflux, feeling gassy
- the risk for perforation of the organ lining (a life-threatening condition requiring emergency surgery to repair small openings in the lining of the GI tract)
- dehydration, weakness and fatigue (if food intake is changed in response to pain when eating)
- diarrhea can occur as a symptom even before other stomach ulcer symptoms start
How long does it take for a stomach ulcer to heal?
Uncomplicated gastric ulcers usually take two or three months to heal. Duodenal ulcers tend to heal quicker than gastric ulcers. While most ulcers are capable of healing, an ulcer can come back if precautions aren’t taken.
Stomach ulcer complications:
Research shows that around 35 percent of patients with ulcers experience other complications besides immediate pain, including the chance for severe perforation of the lining of the GI tract and internal bleeding.
Can you die from an ulcer in your stomach? While ulcers are often pretty painful and can trigger other digestive symptoms, they commonly don’t raise a big risk for death or very serious illnesses. A high percentage of ulcers (up to 90 percent of all cases) can be resolved without the need for surgery or serious medication use.
Peptic ulcers can also play a part in other diseases, particularly diseases related to the liver and kidneys. A stomach ulcer can lead to bleeding in liver cirrhosis and can be a sign of chronic kidney disease.
Diagnosis and Conventional Treatment
If you suspect you have a stomach ulcer, see your doctor to first rule out other causes of your pain. In order to diagnose a stomach ulcer, your doctor may perform an endoscopy, which allows the doctor to view the inside lining of the esophagus, stomach and small intestine.
Once a diagnosis is verified, treatment options can begin.
Your doctor will likely take your medical history and perform a physical exam along with a blood test, plus ask you about your past use of medications and possibly do an X-ray to locate a stomach ulcer. Testing the blood for H. pylori and doing a urea breath test and/or stool test to look for the presence of H. pylori antigens are common ways to diagnose an ulcer.
The goal of stomach ulcer treatments is to help reduce pain and inflammation in the digestive tract, boost the immune system to fight H. pylori bacteria, prevent complications, and lower the chance for future ulcers from forming or returning.
Today, conventional treatment options for stomach ulcers include:
- Stopping use of NSAIDs, alcohol and cigarettes.
- Antacids and acid-reducing medications. Wondering if taking these solves ulcers? Anti-acid medicine may be used for two to six weeks to help healing and relieve pain. Taking antacids for a stomach ulcer might help ease pain temporarily, but it will keep coming back if the underlying issue causing the ulcer isn’t resolved.
- Your doctor might also prescribe other medications to reduce stomach acid and coat and protect your ulcer, such as proton pump inhibitors, histamine blockers, H2-receptor antagonists like Ranitidine or the protectant sucralfate (Carafate). However, ultimately you want to manage your symptoms naturally long term instead of relying on medications since these aren’t always long-term fixes.
- Acid-blocking medications may also be given intravenously in severe cases.
- Antibiotics are sometimes used to control H. pylori, along with acid-suppressing medications, for about two to eight weeks. This combination is sometimes called “triple therapy” or “quadruple therapy.” Once antibiotics are stopped after about two to three weeks, acid-suppressing medications may be taken for up to eight weeks.
- Blood transfusions are used if bleeding due to an ulcer is severe.
- Rarely, surgery may be needed to treat a perforated or bleeding peptic ulcer.
Stomach Ulcer Treatment Plan
1. Boost Immunity Against H. Pylori
Many people host H. pylori in their bodies, but only a minority of people infected with H. pylori develop ulcers. A highly inflammatory lifestyle weakens the immune system and makes the digestive system more susceptible to an infection caused by H. pylori bacterium. H. pylori itself can then cause even more inflammation within the stomach and small intestine, creating a vicious cycle that’s hard to break.
Research shows that today about 30 percent to 40 percent of people in the U.S. get an H. pylori infection, but usually the infection remains dormant, without any noticeable symptoms emerging for years or even ever. Other research suggests that H. pylori is present in more than 90 percent of duodenal ulcers and about 80 percent of stomach ulcers.
H. pylori contributes to ulcers by damaging the mucous coating that protects the lining of the stomach and duodenum from acids. Once damaged, stomach acid is able to get through to the sensitive lining, causing burning and irritation.
H. pylori can be spread through unclean water, food or utensils, plus through bodily fluids (like saliva) — but it’s only likely to cause an ulcer when someone’s immunity is low for other reasons.
Boost protection against infections by dropping poor lifestyle habits like smoking, drinking high amounts of alcohol, eating a poor diet high in processed foods, toxin exposure and a sedentary lifestyle — which favor inflammation, lower immunity and contribute to ulcer formation.
Some of these can also make treatment of ulcers more difficult. For example, research facts show that smoking cigarettes makes ulcers harder to heal and possibly more painful.
You can also protect yourself from H. pylori infection by frequently washing your hands with soap and water and by eating foods that have been cooked completely.
2. Limit Use of NSAID Pain Relievers
People of any age who take NSAIDs every day or multiple times per week are more likely to develop stomach ulcers and heartburn compared to people who don’t take them very often. NSAIDs (like ibuprofen or Advil) are prescribed very often to treat all sorts of conditions that cause a fever, pain and swelling — and some people rely on taking them practically every day to help control their chronic or reoccurring pain (such as headaches, arthritis/joint pain, PMS cramps, muscle tears, infections, colds and so on).
NSAIDs affect the gastrointestinal system by altering how digestive enzymes and stomach acids are produced. There are two enzymes that produce chemicals in your body that promote pain, inflammation and fever. NSAIDs not only decrease these enzymes, but at the same time lower production of another chemical that protects the stomach lining from stomach acid.
NSAIDs also block the formation of some prostaglandins, which usually protect against ulcers.
If you can, stop taking the NSAIDs, or at least greatly reduce how much of them you take regularly. Talk to your doctor about other options for controlling pain.
If you still need NSAIDs, take them with a meal, take a lower dose, or take them along with medications that can protect your stomach and duodenum.
3. Manage Stress
Although the theory that stress alone causes stomach ulcers is no longer fully supported, stress can still play a part in the development of ulcers, and the condition is still considered somewhat “psychosomatic.”
When someone experiences chronic stress, the risk for a stomach ulcer goes up, since there’s a strong “gut-brain connection” involved in normal digestive processes. The body easily picks up on perceived threats and changes how digestion is carried out, which is why a very high percentage of people with anxiety/depression experience some sort of digestive illness or complaints.
People with anxiety and high amounts of stress have been observed to have higher than normal rates of ulcers and more frequent infections caused by H. pylori. Stress weakens the immune system and worsens digestion, making it more likely you become sick from various bacteria or microbes you come into contact with.
In times of high stress, the body uses valuable energy to perform other “life-saving” functions beyond digesting food properly and protecting the body from passing microbes.
To help better manage stress, take advantage of natural stress relievers like regularly exercising, meditating or practicing healing prayer, spending time outdoors, getting good sleep, and using relaxing essential oils for anxiety.
4. Eat a Stomach Ulcer Diet
An improper diet that includes lots of packaged, processed foods and few fresh foods (like vegetables and fruit) raises the risk for ulcers by promoting inflammation and hindering immune functions. Skipping regular meals and eating only one to two times per day, but a large amount of food at once, can also make discomfort and ulcer symptoms worse in some people.
While foods themselves don’t cause ulcers, some people find that eating spicy foods makes their symptoms worse (although this depends on the person and doesn’t affect everyone).
According to the Jackson Seigelbaum Gastroenterology Center, foods most frequently associated with gastric discomfort include:
- black pepper
- red or hot pepper and chili powder
- caffeine
- regular and decaffeinated coffee or tea
- alcohol
- cocoa, chocolate and cola beverages
- citrus fruits and juices
- fatty and fried foods
- tomato products
- peppermint
If your ulcer causes nausea and vomiting, it’s important to prevent dehydration, electrolyte imbalances and nutrient deficiencies. Some people with painful ulcers wind up eating less overall in order to avoid pain/burning and therefore risk not consuming enough calories and nutrients.
The likelihood for inflammation and deficiencies is even higher if the food being consumed is low in vitamins, minerals and antioxidants to begin with.
Other tips related to your diet to help control ulcers include:
- maintaining a healthy weight and avoiding obesity
- avoiding common stomach irritants and allergies to test your reactions (such as gluten and dairy products)
- quitting excessive alcohol use and stopping smoking, since alcohol and smoking irritate the gut lining
- eating smaller meals throughout the day more regularly
- avoiding very hot foods or drinks
- not eating within three hours of bedtime
Final Thoughts
- Estimates show that about 500,000 new cases of peptic ulcers are reported each year in the U.S. alone, and at any given time about 5 million people are affected. In addition, one in 10 adults can expect to deal with painful ulcers at one point or another.
- The most common stomach ulcer symptoms include abdominal pains and burning sensations; bleeding when vomiting or going to the bathroom; nausea and vomiting; darker stool; loss of appetite and changes in body weight; trouble sleeping due to pain; other digestive complaints, like heartburn, acid reflux and feeling gassy; the risk for perforation of the organ lining; dehydration; weakness; and fatigue.
- A high percentage of ulcers (up to 90 percent of all cases) can be resolved without the need for surgery or serious medication use.
- Men develop duodenal ulcers more often than any other kind, including stomach ulcers, contrary to popular belief. On the other hand, the opposite is true for women: They tend to develop more stomach ulcers and fewer ulcers of the duodenal. In general, women are more likely to have ulcers than men, especially if they’re over the age of 70 and take over-the-counter drugs or medications regularly. The peak age for experiencing ulcers is between 55 and 65 years old.
- Stomach ulcer treatments include limiting the use of NSAID pain relievers, managing stress, boosting immunity and controlling inflammation, and eating a low-processed, nutrient-dense diet.












