This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Does Your Shoulder Hurt? Thoracic Outlet Syndrome + 8 Exercises to Help Recovery
June 3, 2018

Between 7 percent to 47 percent of “working age” adults experience shoulder pain at least from time- to-time, especially those who work in office settings and have occupations requiring use of their arms in elevation (like hairdressers/barbers, switchboard operators, assembly line workers, etc.) (1) Although thoracic outlet syndrome (TOS) has always been considered a somewhat “rare” condition that causes shoulder/arm/chest pains, there’s some evidence that it’s become more common over the past several decades. One possible explanation for the rising rates of TOS is that many adults now sit for far too many hours of the day, due to having sedentary “desk jobs.” Sitting all day is problematic on its own, but most people also have poor posture, contributing to tightness and also certain chronic diseases.
On the other hand, TOS can also affect athletes and certain types of manual labor workers who use their arms and hands in repetitive ways — including weight-lifters, cyclists, pitchers, construction workers, etc. These groups of people are at an increased risk for thoracic outlet syndrome symptoms including tingling in the hands, weakness in the arms, neck straining, and collarbone or shoulder pain.
What can be done for thoracic outlet syndrome? Physical therapy, specific stretches and regular exercise are key components of thoracic outlet syndrome treatment. Other steps that can help to prevent and treat TOS include fixing your workstation setup, improving your posture, stretching regularly, and eating an anti-inflammatory diet.
What Is Thoracic Outlet Syndrome?
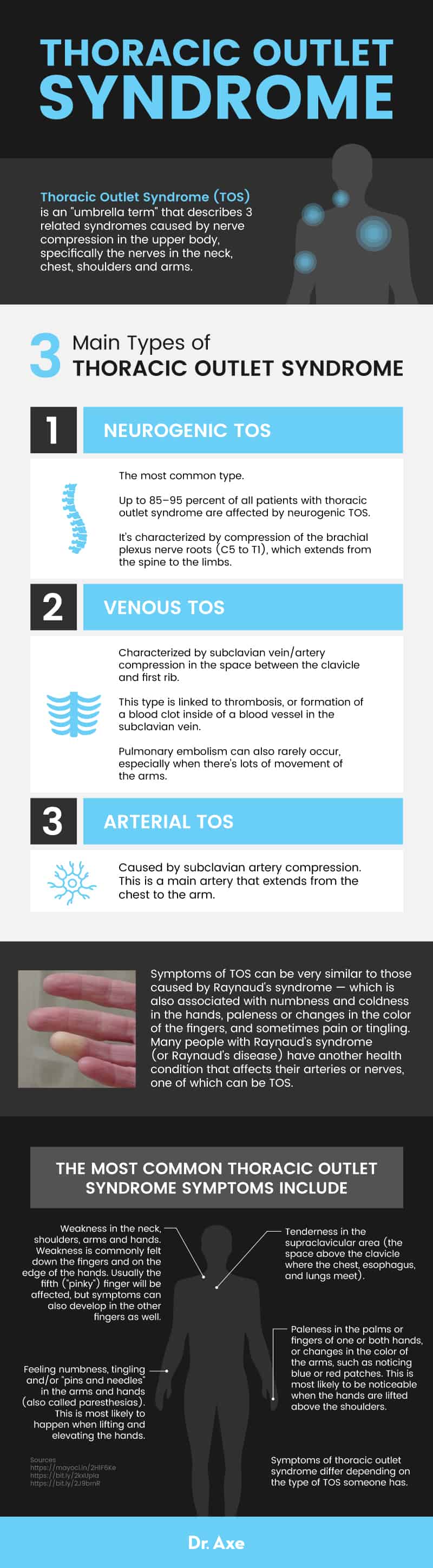
Thoracic Outlet Syndrome (TOS) is an “umbrella term” that describes three related syndromes caused by nerve compression in the upper body, specifically the nerves in the neck, chest, shoulders and arms.
Technically, thoracic outlet syndrome is brought about by abnormal compression of the thoracic outlet (the space between your collarbone and your first rib and the neurovascular bundle of small bones, ligaments and muscles in the cervical spine and the lower axilla (the armpit, or the space below where the shoulder vessels and nerves enter the upper arm). (2) It’s a common reason that people experience numbness and tingling down either one or both of their arms and/or hands.
There are 3 main types of thoracic outlet syndrome: neurogenic, vascular and arterial TOS. (3)
- Each type of TOS causes somewhat unique symptoms, although there is lots of overlap between the different types.
- Neurogenic TOS is the most common, followed by venous, and then arterial. Up to 85–95 percent of all patients with thoracic outlet syndrome are affected by neurogenic TOS. (4) This type is characterized by compression of the brachial plexus nerve roots (C5 to T1), which extends from the spine to the limbs.
- Venous TOS is characterized by subclavian vein/artery compression in the space between the clavicle and first rib. This type is linked to thrombosis, or formation of a blood clot inside of a blood vessel in the subclavian vein. Pulmonary embolism can also rarely occur, especially when there’s lots of movement of the arms.
- Arterial TOS is caused by subclavian artery compression. This is a main artery that extends from the chest to the arm.
Symptoms of TOS can be very similar to those caused by Raynaud’s syndrome— which is also associated with numbness and coldness in the hands, paleness or changes in the color of the fingers, and sometimes pain or tingling. Many people with Raynaud’s syndrome (or Raynaud’s disease) have another health condition that affects their arteries or nerves, one of which can be TOS.
Symptoms
The most common thoracic outlet syndrome symptoms include: (5)
- Tenderness in the supraclavicular area (the space above the clavicle where the chest, esophagus, and lungs meet).
- Feeling numbness, tingling and/or “pins and needles” in the arms and hands (also called paresthesias). This is most likely to happen when lifting and elevating the hands.
- Weakness in the neck, shoulders, arms and hands. Weakness is commonly felt down the fingers and on the edge of the hands. Which fingers are affected by thoracic outlet syndrome most? Usually the fifth (“pinky”) finger will be affected, but symptoms can also develop in the other fingers as well.
- Paleness in the palms or fingers of one or both hands, or changes in the color of the arms, such as noticing blue or red patches. This is most likely to be noticeable when the hands are lifted above the shoulders.
Symptoms of thoracic outlet syndrome differ depending on the type of TOS someone has.
- Neurogenic TOS (also called Gilliatt-Sumner hand) causes severe wasting in the fleshy base of the thumb. It can also cause pins and needles, changes in hand color including paleness/white hands, cold in the hands, dull aching pains in the neck, and pain in the shoulders and near the armpits.
- Venous TOS (in which Paget-Schroetter syndrome is a subset) causes paleness/pallor in the hands, a weak pulse in the affected arm, coldness in the hands, numbness, tingling, aching, swelling of the fingers, and weakness of the neck or arms.
- Arterial TOS causes the most noticeable changes in color and cold sensitivity in the hands and fingers. It can also cause swelling, tenderness, heaviness, and poor blood circulation in the arms, hands, and fingers.
Causes and Risk Factors
Among doctors who specialize in treating conditions such as TOS, there is still some ongoing debate about the exact physiological causes of the condition. Many agree that TOS is tied to compression of the brachial plexus or subclavian vessels that run down the neck to the armpit and arms. (6) The nerves that lead to the arms come from the spine out through the neck, through the shoulders and to the arms. They can become irritated and strained due to poor posture, repetitive movement and for other reasons. Compression occurs when the size and shape of the thoracic outlet is altered. This can be caused by a number of different factors, depending on the person’s overall health and genetics.
Can trauma cause thoracic outlet syndrome? Yes, physical trauma is one of the most common thoracic outlet causes. For example, symptoms can be due to an accident, a surgical procedure, or after developing frostbite. Other reasons someone can develop TOS include:
- History of injuries affecting the neck, arms and hands.
- Poor posture that causes nerve compression, especially forward head posture which strains the neck.
- Doing repetitive arm and shoulder movements. This can include movements involved in certain lines of work, or the types done during exercise, when playing sports, or during other physical activities.
- Being born with anatomical defects that cause nerve compression.
- Tumors that press on nerves.
- Pregnancy.
Who’s at the greatest risk of developing thoracic outlet syndrome? TOS risk factors include:
- Being a woman, since women are affected more often than men.
- Being between the ages of 20 and 50 years of age, which is when symptoms usually start.
- Living a sedentary lifestyle, with too little physical activity.
- Being a high-level athlete, especially regularly playing baseball, softball, wrestling, swimming, hockey, martial arts, backpacking, and billiards (all of these have been linked to venous TOS). (7)
- Dealing with chronic stress, which can increase tension in the neck.
- Obesity or being very overweight.
- History of diabetes, neuropathy and other nerve-related conditions.
- Sleep deprivation and depression, which cause tightened muscles and worsen inflammation/pain.
- Smoking and high alcohol consumption.
- Symptoms may be made worse by taking certain medications that cause the arteries to narrow and reduce blood flow. These can include: beta blockers, birth control pills, allergy medications, diet pills, migraine medications that contain ergotamine, and some cancer medicines, including cisplatin and vinblastine.
Conventional Treatment
What does research suggest about thoracic outlet syndrome prognosis? Most people with TOS will find relief from symptoms if they follow an exercise and physical therapy program that addresses compression of their nerves and arteries. However, some people with more severe cases of TOS, especially vascular and neurogenic TOS, may need to use medications or undergo surgery to recover.
It’s important to talk to your doctor about any TOS symptoms you might be experiencing in order to get an accurate thoracic outlet syndrome diagnosis. Keep in mind that there are many other conditions and disorders that affect the nerves and blood vessels in the upper body that can cause similar symptoms to TOS. For example, your symptoms may actually be due to:
- Raynaud’s disease/Raynaud’s syndrome
- Frozen shoulder
- Cervical disc disorders
- Rotator cuff injuries
- Fibromyalgia
- Multiple sclerosis
- Complex regional pain syndrome
- Tumors of the syrinx or spinal cord
If your doctor suspects you may have TOS, he or she will likely want to perform several thoracic outlet syndrome tests. TOS can be diagnosed following a physical exam that reveals tenderness in the supraclavicular area, weakness in the upper body, and/or “pins and needles” down the arms. Your doctor will also want to discuss your medical history, exercise routine, and any other symptoms you’re experiencing. Based on your symptoms, he or she might recommend you have other tests completed to rule out or diagnose TOS, such as conduction studies, electromyography, or imaging studies.
Treatment options for thoracic outlet syndrome can include one or more of the following:
- Exercise program used to strengthen and stretch muscles in the chest, shoulders and neck.
- Physical therapy to help restore normal posture, strengthen key muscles, and relieve compression in affected nerves. Heat may also be used to assist stretches/exercises since it relaxes muscles.
- Use of non-steroidal anti-inflammatory drugs (NSAIDs) to help decrease pain.
- Use of anticoagulants and thrombolytic medications, which are used to prevent and break up blood clots.
- Rarely, surgery may also be recommended if other treatment options don’t work to relieve symptoms. What procedure is performed to relieve thoracic outlet syndrome? The goal of TOS surgery is decompression/release of the affected nerves or arteries.
Stretches and Exercises
Below you’ll find thoracic outlet syndrome exercises that experts recommend you ideally perform daily to help manage your symptoms. Always perform TOS exercises slowly and carefully so you don’t strain yourself and cause more pain. The goal is to perform upper body and shoulder exercises to help strengthen your chest and to stretch tight areas to the point where a stretch is felt intensely but that you are not feeling pain.
Hold each stretch below for 30 seconds and then release slowly. Take about 10 seconds between each stretch to rest. Repeat all stretches ideally about three to five times. (8, 9)
1. Back of Neck Stretch — Sitting or standing, interlace your fingers behind your head. Gently lean your head back with support from your hands as you lift your chest, then reverse and tuck your chin to your chest. Move slowly and back and forth while you breathe.
2. Side of Neck Stretch — Sit down in a chair and place your affected hand behind your head. Turn your head away from the tight side, look down until a slight stretch is felt. Take a deep breath, exhale slowly while holding.
3. Chest Stretch — Sit in a sturdy chair next to a table. Place your arms on the table straight in front of you. Lean forward while bending at the waist as far as possible while you extend your head and chest forward.
4. Shoulder Stretch — Stand with your back to a table and wrap your arms backwards to try and grasp the edge of the table with your fingers. While facing forward, slowly bend your knees and allow your elbows to bend.
5. Pectoralis Stretch — Stand in an open doorway and lift your hands above your head to reach near the door frame. Slowly lean forward until you feel a stretch in the front of your shoulders.
6. Rowing Exercise — Wrap an exercise band/tube around an immovable object. Hold one end of the band in each hand. Sit in a chair, bend your arms 90 degrees, and pull backward on the band as you squeeze your shoulder blades together. Try to complete two sets of 15.
7. Mid-Trap Exercise — Lie on your stomach and place a folded pillow underneath your chest. Place your arms out straight to your sides with your elbows straight and thumbs pointing up. Slowly raise your arms toward the ceiling as you squeeze your shoulder blades together (like you were squeezing an orange between your shoulders). Try to complete three sets of 15.
8. Flys — Hold a light dumbbell in each hand near the hips while standing straight, than raise the weight sideways a few inches away from the body with straight arms. Lift your arms away from your body out to the side, forming an upside down “V” shape. Bring the weights back towards the hips and repeat about 10 to 12 times. If it feels more comfortable, you can also perform flys while sitting, or with bent arms (sometimes called a “bent arm lateral raise”).
The best way to add strength to your upper body is to do exercises that target different parts of the shoulders, chest and arms. As long as you’re not in pain, this can be done using various types of body moves, dynamic motions and weighted exercises. Here’s a list of exercises that can be incorporated into your workouts to improve range of motion and strength:
- Variations of planks
- All types of push-ups, including TRX push-ups
- Rowing exercises
- Overhead presses
- Cable pulls
- Flys
- Lateral raises
- Yoga moves that involve holding up the weight of the upper body
Prevention
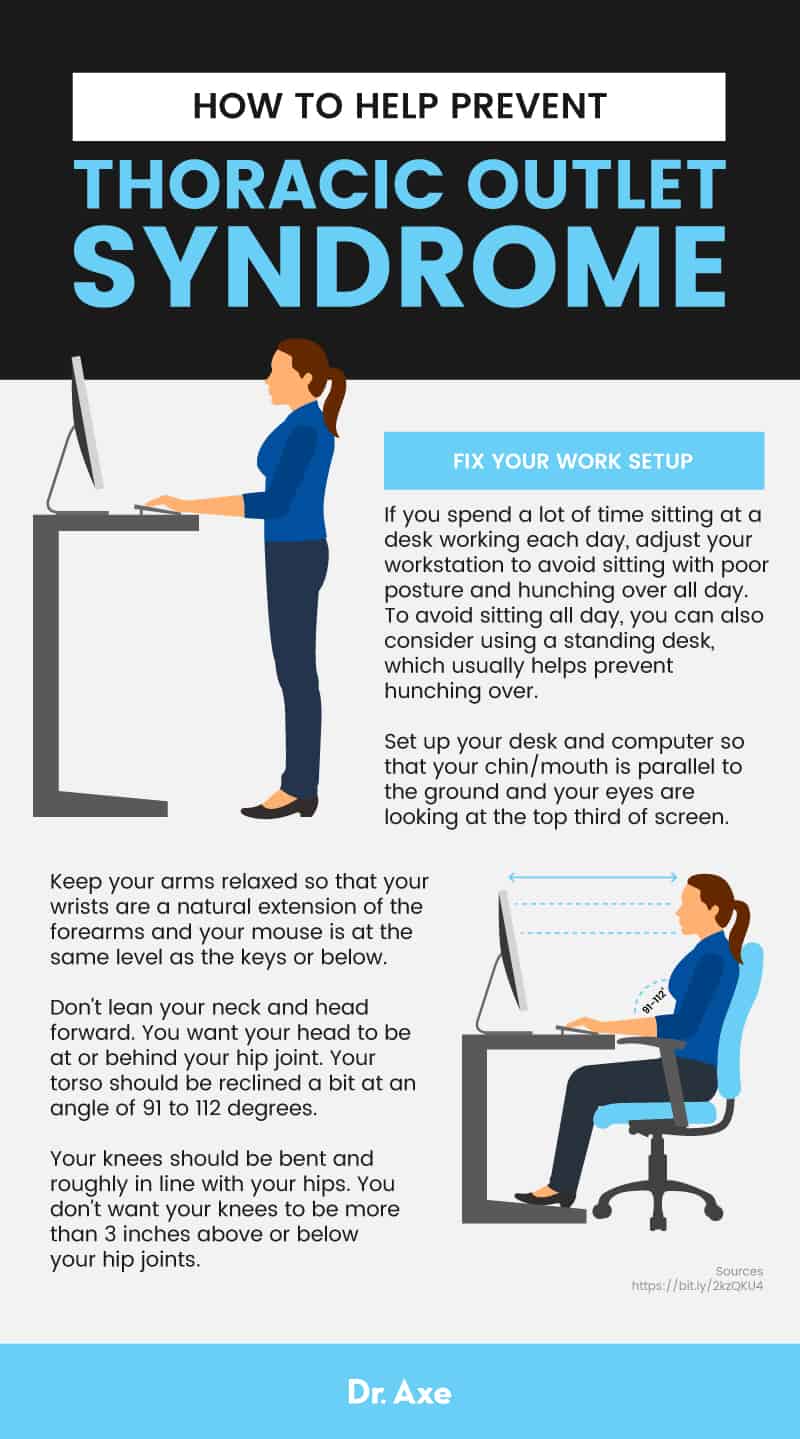
1. Fix Your Work Setup
If you spend a lot of time sitting at a desk working each day, adjust your workstation to avoid sitting with poor posture and hunching over all day. (10) This is important because poor posture can cause problems relating to inadequate blood supply to the arms over long periods. To avoid sitting all day, you can also consider using a standing desk, which usually helps prevent hunching over.
- Set up your desk and computer so that your chin/mouth is parallel to the ground and your eyes are looking at the top third of screen.
- Keep your arms relaxed so that your wrists are a natural extension of the forearms and your mouse is at the same level as the keys or below.
- Don’t lean your neck and head forward. You want your head to be at or behind your hip joint. Your torso should be reclined a bit at an angle of 91 to 112 degrees.
- Your knees should be bent and roughly in line with your hips. You don’t want your knees to be more than three inches above or below your hip joints.
2. Manage Stress
Stress can worsen thoracic outlet syndrome symptoms, increasing muscle tension and tightness. Emotional or physical stress can cause vasoconstriction, further negatively impacting blood flow.
- Try stress relievers like practicing yoga, taking walks outside, or taking time to do meditation or devotional prayer each day.
- If you’re dealing with a lot of emotional stress, you might also consider cognitive behavioral therapy or joining a support group.
- Acupuncture may be helpful in reducing stress-related symptoms including pain, inflammation and joint stiffness.
- Use calming essential oils like lavender, ylang ylang and chamomile oil.
- Try mind-body practices like spinal manipulation, meditation, reiki, guided imagery, deep breathing exercises and other relaxation techniques.
3. Give Yourself Enough Recovery Time
Exercise is beneficial in numerous ways, but overtraining can contribute to TOS — especially if you exercise with poor form and don’t leave enough time between workouts for your muscles and joint to heal. Take breaks from repetitive exercises or movements that are contributing to your symptoms. Give yourself two days between tough workouts to properly recover. One effective way to do this is to focus on different muscle groups each workout so that you rotate body parts.
I also recommend doing foam rolling/using a spikey ball to help keep muscles loose. Massage therapy, working with a physical therapist, and visiting a chiropractor are other options if you struggle with poor form, reduced range of motion and lots of tightness. One therapy that can help is dry needling.
4. Reduce Inflammation
- Quit smoking and avoid consuming too much alcohol.
- Remove inflammatory foods from your diet, including those with added sugar, processed oils, refined carbohydrates, artificial ingredients and chemicals, alcohol and even caffeine. Instead fill up on anti-inflammatory foods like: green leafy vegetables, berries, wild-caught salmon and bone broth, nuts and seeds, good quality organic meats, fresh vegetables and spices and herbs.
- Avoid very hot or cold temperatures that might worsen symptoms like tingling and color changes in your hands.
5. Check Your Medications
If you are taking any medication that can lead to reduced blood flow, this may contribute to TOS. Talk to your doctor about some alternatives.
Precautions
If you’re treating thoracic outlet syndrome for the first time, I recommend you consult a physician before beginning any treatment program. Be sure to rule out any other conditions that may be causing you pain and discomfort. If you notice symptoms getting worse when you begin exercising and stretching, always be sure to stop and see your doctor for help.
Final Thoughts
- Thoracic Outlet Syndrome (TOS) is an “umbrella term” that describes three related syndromes caused by nerve compression in the upper body, specifically the nerves in the neck, chest and arms.
- The three types of TOS are: neurogenic, vascular and arterial. Neurogenic is by far the most common type.
- Thoracic outlet syndrome symptoms include: tenderness, numbness, tingling and/or “pins and needles” in the arms and hands (also called paresthesia); weakness in the neck, shoulders, arms and hands; paleness or changes in color of the fingers; pain, swelling and sensitivity in the upper body.
- There are many different thoracic outlet syndrome causes, some of which can include: injuries affecting the neck, arms and hands; poor posture that causes nerve compression; repetitive arm and shoulder movements, doing certain repetitive exercises; anatomical defects; tumors that press on nerves; and pregnancy.
- Exercises and physical therapy are recommended treatments for TOS. Some may also need medications to control pain or blood clots, and, rarely, surgery.
Read Next: 11 Natural Treatments for Rotator Cuff Pain + Best Rotator Cuff Exercises