This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Perimenopause Symptoms You Can’t Ignore & What to Do About Them
February 2, 2023

When women reach a certain age, menopause symptoms begin to show themselves, sometimes even before hitting menopause. This is called perimenopause, and perimenopause symptoms can be just as challenging to deal with.
While perimenopause and menopause are both natural parts of aging, and therefore not necessarily “problems to solve,” it’s normal and expected to experience changes and certain symptoms during this transition. Just as with pregnancy, labor and other reproductive changes (even puberty), taking steps to manage your expectations and lower symptoms can help make this sometimes unpredictable time period a bit easier.
Not every woman going through the stages of menopause experiences side effects or any decrease in quality of life, but a majority do. In particular, the perimenopause years are when estrogen and progesterone fluctuate the most in the female brain.
The degree to which you struggle with perimenopause symptoms and menopause has a lot to do with several factors that make your body unique, including your personal medical history, genetics, the quality of your diet, how active you are and your stress levels.
By making certain lifestyle changes before and during the phases of menopause — for example, regarding the foods you choose to eat (and don’t eat), herbal medicines or supplements you take, and stress-reducing practices you make apart of your regular routine — you’re likely be able to find some relief from menopause and perimenopause symptoms and better handle the hormonal changes associated with this important time of life.
What Is Perimenopause?
A women’s reproductive life is split into three major time periods:
- Active reproduction/fertility
- Menopausal years (including perimenopause)
- Postmenopause years
The process that most people refer to as “menopause” can actually be divided into three parts: perimenopause, menopause and postmenopause. Menopause is defined as the time period that starts 12 months after a woman’s last menstrual cycle/last period. Perimenopause is considered the time period before menopause starts, prior to the “cessation of periods for 12 consecutive months.” For some women, perimenopause can come on so gradually and in the midst of many other life changes that perimenopause symptoms mostly go unnoticed, even for several years.
When does perimenopause begin? Just like with menopause itself, this differs from woman to woman. While life expectancy has increased over the years, the average age of menopause has not changed during the past few centuries. However, some women are now beginning perimenopause earlier due to having certain medical problems in the past.
Perimenopause usually starts sometime during a woman’s mid-40s and can last for several years (in some cases even longer, such as up to 10 years). It’s common during this time to experience irregular periods, breakthrough bleeding and other signs that reproductive hormones are shifting.
Then menopause usually officially begins between the ages of 44–55 (the average age in the U.S. is 51). Once a woman fully stops releasing eggs from her ovaries and no longer has a period for one full year, then she has officially entered menopause and is no longer in perimenopause.
How is perimenopause different from “premenopause”? These two terms are often used interchangeably to describe the same time period prior to menopause. However, premenopause technically is any time prior to entering menopause, while perimenopause is the several-year period right before menopause starts.
Premenopause includes all years after a woman has begun menstruation but before her periods stop all together. This means premenopause should be used to refer to any woman, any time before menopause has occurred and fertility/reproductivity is still active, which can include perimenopause.
In other words, it’s possible to be in your 20s or 30s and “premenopausal” but not yet consider yourself to be in the perimenopause phase. Some also use the term “premature” to describe the time period after 40 years old but before perimenopause has started.
Symptoms
During perimenopause, ovarian function and estrogen production start to become erratic, and therefore a woman’s cycle is usually somewhat unpredictable. It’s common for many women starting in their early 40s to begin noticing signs of perimenopause, including perimenopause symptoms like menstrual changes, weight gain (especially in the abdomen), decrease in breast volume, hair thinning and skin dryness. Other physical signs, such as irregular vaginal bleeding and hot flashes, might start to come and go even earlier, starting in the late 30s.
The most common signs and perimenopause symptoms include:
- Menstrual changes and irregular periods: Periods tend to occur every two to four months on average at first, and then further and further apart. Periods can also get heavier or lighter at times.
- Hot flashes and night sweats: This feels like heat suddenly starting to spread throughout the body, often causing sweating and redness. A “hot flush” is the term given to the redness that’s caused by an increase in body temperature. These perimenopause symptoms are caused by hormonal changes mostly affecting the hypothalamus, which controls body temperature.
- Insomnia and changes in sleep quality: Many women start to have trouble getting good sleep and might start to wake up sweaty and hot.
- Gradual weight gain: As the metabolism slows down, muscle mass is reduced and bones start to become less dense, it’s common to gain some weight (especially in the stomach). Exercise and a healthy diet are more important during this time than ever.
- Changes in sex drive: A decrease in estrogen causes blood flow to be reduced to the genital area. Throughout the menopausal years, the labia becomes smaller, and the muscle tissue of the clitoris starts to shrink and become less sensitive. There are also many changes taking place in the uterus, ovaries and cervix (becoming smaller and narrower).
- Vaginal dryness and changes: The vagina technically shortens and loses elasticity (called vaginal atrophy). Vaginal thinness and dryness can come along with higher susceptibility to urinary tract infections caused by vaginal fluid loss/less lubrication to move bacteria out.
- Increased abdominal fat and weight gain: Due to a slowed metabolism.
- Thinning hair and dry skin: Many women notice their skin starting to show signs of aging, such as wrinkles, dark spots, dryness, less elastic and sometimes more itchiness.
- Changes in breast tissue: The breasts might start becoming smaller, less dense, have more fatty tissue and lose some of their volume (becoming “saggier”).
- Mood swings: This can include feeling like you’re always tired, increased irritability, anxiety, fatigue or depressive symptoms. Perimenopausal women have been found to have higher than normal levels of MAO-A, the enzyme that breaks down serotonin, norepinephrine and dopamine and is linked to major depressive disorder and postpartum depression.
- Heart palpitations: This is caused by changes to the blood vessels, heart and autonomic nervous system. Palpitations might occur during hot flashes or with anxiety, muscle spasms and headaches.
- Migraines and frequent headaches: Reduced blood flow, lack of sleep, anxiety and other problems can contribute to frequent headaches.
- Poorer concentration: Estrogen and testosterone play a role in memory, motivation and mood. It’s common to start noticing loss of concentration, forgetfulness, drowsiness and increased reactions to stress. These perimenopause symptoms can also be worsened due to poor sleep and increased anxiety.
- Higher risk for other diseases and complications: Studies show that during menopause and afterward, a woman’s risk for heart and blood vessel (cardiovascular) diseases, as well as osteoporosis, increases. This is due to a decline in estrogen levels, which changes fat accumulation and also contributes to loss of bone density, weak bones and increased risk of fractures. Some experts argue that the increased risk might be related more to general effects of aging rather than menopause itself, but estrogen loss has been shown to be tied to these conditions over and over again.
Causes
During each of the major reproductive phases of a woman’s life described above, various hormonal glands in her body work together to control how much of each hormone is produced. Glands including the pituitary, ovaries and thyroid all play a role in the transition into menopause. Even other organs/tissue such as the uterus, breast tissue and fat cells (adipose tissue) are capable of secreting hormones that influence reproduction.
The major hormonal changes involved in perimenopause, menopause and postmenopause include estrogen, progesterone and testosterone. While other hormones are also usually shifting and involved (including serotonin and insulin), these three have the biggest influence over a woman’s reproductive capabilities — especially estrogen.
- Estrogen is the collective term for three types of female hormones (estoril, estradiol and estrone) that are mostly secreted by the ovaries. The three types of estrogen are primarily responsible for giving a woman her female qualities (and to some degree men too), including her reproductive capabilities, fat around her hips/thighs and her smooth skin.
- Progesterone is the hormone that prepares the uterus for pregnancy in addition to having other jobs, and testosterone is the hormone mostly associated with masculine qualities.
- When your ovaries stop making a high percentage of your body’s estrogen (they’re responsible for 90 percent of production prior to menopause), you enter menopause. Because estrogen has important effects on your bodyweight and composition, mood, sleep, sex drive, cognitive function, memory, and blood flow, many different symptoms can be experienced during perimenopause/menopause as a result of decreasing estrogen levels.
- Can you still become pregnant during perimenopause, you might be asking yourself? Technically, yes, you can. Although the menstrual cycle is irregular and fertility at this time in a woman’s life is low, it’s not impossible to become pregnant until entering menopause.
Facts
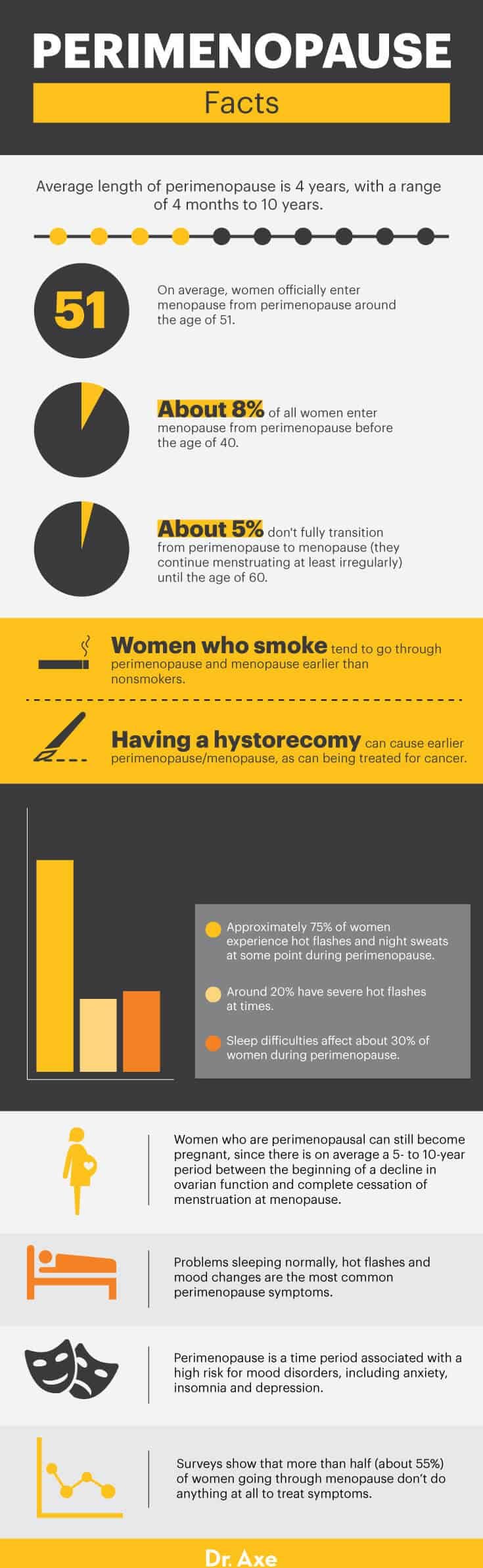
- The average length of perimenopause is four years, with a range from about four months up to 10 years. In contrast, the average duration of menopause is 2.5 to three years but sometimes up to 10.
- On average, women officially enter menopause from perimenopause around the age of 51.
- About 8 percent of all women enter menopause from perimenopause before the age of 40. About 5 percent don’t fully transition from perimenopause to menopause (they continue menstruating at least irregularly) until the age of 60.
- Women who smoke tend to go through perimenopause and menopause earlier than nonsmokers do. Having a hysterectomy also causes earlier perimenopause/menopause, as can being treated for cancer.
- Problems sleeping normally, hot flashes and mood changes are the most common perimenopause symptoms. Approximately 75 percent of women experience hot flashes and night sweats at some point during perimenopause. Around 20 percent have severe hot flashes at times.
- Sleep difficulties affect about 30 percent of women during perimenopause. Trouble sleeping is one of the earliest signs of changing hormones and can begin in the late 30s.
- Perimenopause is a time period associated with a high risk for mood disorders, including anxiety, insomnia and depression.
- Women who are perimenopausal can still become pregnant, since there is on average a five- to 10-year period between the beginning of a decline in ovarian function and complete cessation of menstruation at menopause.
- Research has not revealed any link between the age of natural menopause and use of oral contraceptives in the past, socioeconomic or marital status, race, or age when a woman’s menstrual cycle began.
- Research shows that more than half of women going through menopause seek some sort of menopause treatment to deal with symptoms.
- Research shows that gradual estrogen loss can increase the risk of certain diseases, such as osteoporosis and sarcopenia. Approximately 80 percent of Americans with osteoporosis or low bone mass are women, and about half of all women older than 50 suffer an osteoporosis-related bone fracture in their lifetimes.
Perimenopause vs. Menopause
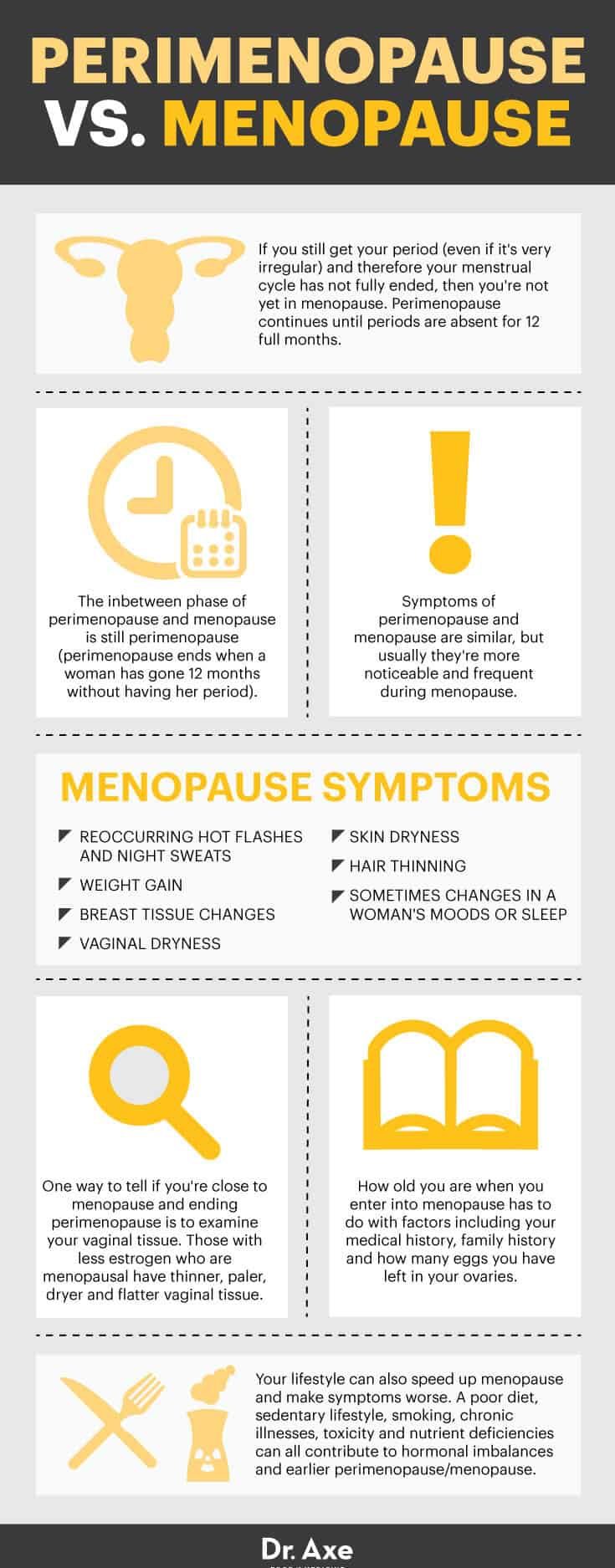
- If you’re still getting your period (even if it’s very irregular) and therefore your menstrual cycle has not fully ended, then you’re not yet in menopause. Perimenopause continues until periods are absent for 12 full months.
- The in-between phase of perimenopause and menopause is still perimenopause (perimenopause ends when a woman has gone 12 months without having her period).
- Symptoms of perimenopause and menopause are similar, but usually they’re more noticeable and frequent during menopause.
- Menopause symptoms often include reoccurring hot flashes and night sweats, weight gain, breast tissue changes, vaginal dryness, skin dryness, hair thinning, and sometimes changes in a woman’s moods or sleep.
- One way to tell if you’re close to menopause and ending perimenopause is to have your gynecologist examine your vaginal tissue. Those with less estrogen who are menopausal have thinner, paler, dryer and flatter vaginal tissue.
- How old you are when you enter into menopause has to do with factors including your medical history, family history and how many eggs you have left in your ovaries.
- Your lifestyle can also speed up menopause and make symptoms worse. A poor diet, sedentary lifestyle, smoking, chronic illnesses, toxicity and nutrient deficiencies can all contribute to hormonal imbalances and earlier perimenopause/menopause.
Conventional Treatment
The most common conventional treatments for managing menopause or perimenopause symptoms include:
The reason some women turn to these treatments is that they can help mimic or replace some of the decreasing reproductive hormones (such as estrogen or progesterone) and therefore diminish some symptoms of menopause. Unfortunately, these treatments also pose risks. Studies show that taking hormone replacement therapies can increase a woman’s risk for several serious diseases, including:
- Breast cancer
- Heart disease
- Stroke
- Blood clots
- Urinary incontinence
- Dementia and memory loss
Some experts state that these risks are statistically insignificant, however, and that hormone replacement therapy is worth pursuing as soon as the menopausal symptoms begin to appear. The purpose of hormone replacement therapy is to restore female hormone levels, which can bring relief.
Natural Remedies
1. Healthy Diet
A nourishing, unprocessed diet is key for boosting your intake of essential nutrients, helping your body adjust to changing hormones, managing your weight and reducing your intake of empty calories.
Foods that are most helpful during menopause include organic fruits and veggies, high-fiber foods like nuts and seeds, omega-3 foods, probiotics, clean and lean proteins like fish or grass-fed meat, healthy fats such as olive and coconut oil, and foods that supply natural phytoestrogens, including flax and fermented soy.
In particular, cruciferous vegetables such as broccoli, cabbage and kale contain indole-3-carbinol, which naturally helps to balance estrogen levels.
Fiber is important for cardiovascular and digestive health, plus maintaining a healthy weight. Some studies have even found that diets higher in fiber might help to balance production of estrogen.
Studies show that frequently consuming omega-3s facilitates in hormone production and might help to prevent menopausal problems, postmenopausal osteoporosis, heart complications, depression and breast cancer.
During perimenopause, some studies suggest beginning to increase phytoestrogen intake to counteract the effects of the hormonal imbalances women begin to experience. Some research indicates a drastic drop it in hot flashes for women in perimenopause eating a phytoestrogen-rich diet.
Another benefit phytoestrogens may offer to menopausal or postmenopausal women is a reduction in bone loss, leading to higher bone density and fewer breaks, when administered in dose-specific measures alongside vitamin D. Research also indicates that phytoestrogens improve heart health, specifically in postmenopausal women.
And don’t forget about water. Aim for eight glasses daily to help replace fluid lost from hot flashes and to decrease bloating.
2. Exercise
Keeping up with an exercise routine consisting of aerobic and strength-training exercise at least three or more times per week can result in improvements in bodyweight, sleep quality, insomnia or depression symptoms, bone density, muscle mass and inflammation.
Even if you haven’t been active in the past, it’s never too late to start getting the benefits of exercise.
3. Supplements and Herbal Treatments
Menopause supplements and herbs that can help mitigate certain symptoms of perimenopause (such as anxiety, fatigue, hot flashes and sleep-related problems) include omega-3 fatty acids, adaptogen herbs such as maca or American ginseng, black cohosh, red clover, raspberry leaf, vitex and St. John’s wort.
For example, studies have focused on use of black cohosh for managing menopause symptoms, especially hot flashes. While findings have been mixed, many feel there is little doubt that black cohosh is a natural remedy for menopause relief. Certain systematic reviews and studies have found that taking it regularly typically reduces the number and severity of negative symptoms that often overwhelm women with hormone problems.
Vitex (or chasteberry) is often combined with other herbs, such as black cohosh or dong quai, for maximum benefits. One study published in Gynecological Endocrinology found that an herbal supplement containing chasteberry provided safe and effective relief of hot flashes and sleep disturbances in pre- and postmenopausal women. Another study found that a supplement containing Vitex as a key ingredient was able to reduce moderate to severe menopausal symptoms.
St. John’s wort uses include being tested as an herbal remedy that relieves the psychological and vegetative symptoms of menopause. A study published in Advance in Therapy and performed in Berlin investigated 12 weeks of treatment with St. John’s wort; 111 women, ages 43 to 65, took one 900 milligram tablet three times daily. All of the participants experienced symptoms characteristic of the pre- and postmenopausal state.
Substantial improvement in psychological and psychosomatic symptoms was observed, and menopausal complaints diminished or disappeared completely in 76 percent of the women; in addition to this, sexual well-being also improved after treatment.
4. Getting Proper Sleep
Sleep is important for restoring energy, balancing hormones, keeping cortisol levels under control, and reducing anxiety or depression. Aim for seven to nine hours a night.
If you have trouble sleeping (as many perimenopausal women do), try using hormone-balancing essential oils such as lavender, reading or writing in a journal, taking magnesium supplements, using Epsom salts in a warm bath prior to bed, turning down the temperature in your room, and practicing mind-body practices such as yoga and meditation.
5. Stress-Reducing/Mind-Body Practices
Because sleep problems, anxiety, fatigue and depression tend to climb during the transition into menopause, it’s important to manage stress as best you can. Ways to do this include natural stress relievers like exercising, spending time outdoors, meditation or prayer, seeking social support, joining a helpful cause or volunteering, reading something inspirational and uplifting, and doing something creative.
6. Gua Sha Therapy
Gua sha is an ancient Chinese therapy that uses a tool to rub or scrape the skin’s surface in long strokes. A study researched gua sha as a potential remedy for perimenopause and found that it was effective as well as safe in helping to relieve symptoms, plus improving the quality of life for the participants.
Precautions
It’s important to see a specialist or to consult with a doctor, even about natural remedies for perimenpause symptoms, if any of the following apply to you:
- You’ve gone six months or more without any sign of bleeding or a menstrual cycle, but then have spotting. Although it’s rare, this sometimes can be a sign of other serious conditions that should be checked out, including uterine cancer or hyperplasia.
- You have a history of breast cancer, ovarian cancer, endometriosis or blood clots. If you have a strong family history of these conditions, it’s also a good idea to be closely monitored.
- You’ve had a hysterectomy, ovarian dysfunction or other serious problems associated with reproductive health.
- You’ve experienced side effects from taking either hormone replacement therapy drugs, birth control pills or herbal treatments in the past.
Final Thoughts
- Perimenopause is the time period prior to the official start of menopause, which begins when a woman has not had her period for one full year.
- Symptoms of perimenopause include hot flashes, problems sleeping normally, increased depression or anxiety, menstrual irregularity, and vaginal changes.
- Perimenopause symptoms usually last around four years but can sometimes come and go for up to 10 years before menopause begins.
- Natural remedies and treatments for perimenopause symptoms include a healthy diet, exercise, supplements, herbal treatments and stress reduction.








