This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Coronary Artery Disease: 6 Natural Ways to Help Beat CAD
June 17, 2018

“Coronary” means around the heart. Coronary artery disease (CAD) occurs when the major blood vessels around your heart become diseased. The disease also affects the heart itself, so it is important to take steps to prevent the damage from becoming serious, which can be life-threatening. (1)
What Is Coronary Artery Disease?
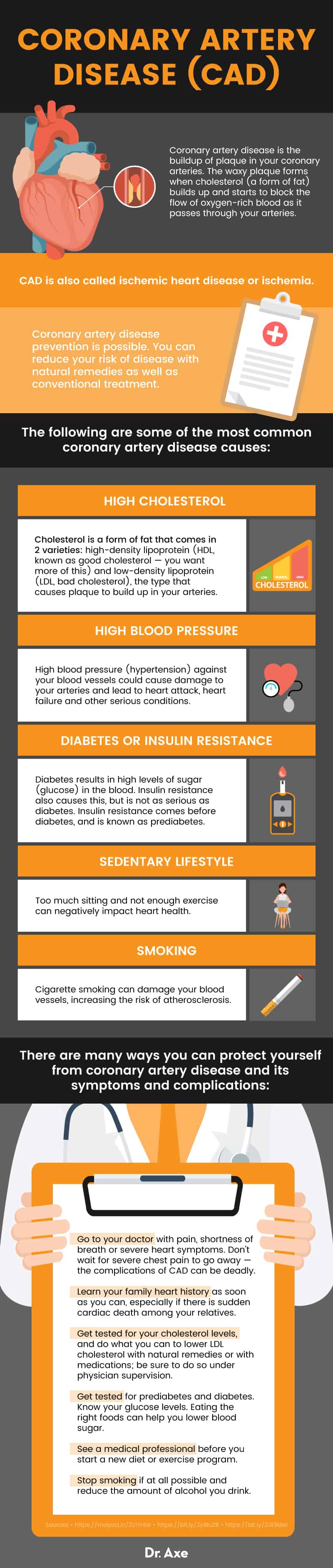
Coronary artery disease (CAD) refers to the buildup of plaque in your coronary arteries. The waxy plaque forms when cholesterol (a form of fat) builds up and starts to block the flow of oxygen-rich blood as it passes through your arteries.
Over time, this can greatly reduce blood flow through your arteries, and the risk of a serious outcome grows. (1)
What Is Heart Disease?
You may have heard the term coronary heart disease (CHD), too. CHD is a result of coronary artery disease. CHD refers to what may happen to your heart after coronary artery disease develops. This article will discuss your artery health as it relates to your heart health. CAD is also called ischemic heart disease or ischemia. (2)
CAD or ischemia is more common in people with diabetes. (3)
Several major types of problems can occur as a result of CAD: (4)
- Stable angina — Stable angina is chest pain or discomfort caused by the poor flow of blood through your coronary arteries into your heart muscle. The chest pain may not be too intense or too frequent.
- Unstable angina — This form of angina is more dangerous than stable angina because it happens when the blockage in your arteries grows to the point that your heart doesn’t get enough oxygen. Unstable angina raises your risk for a heart attack.
- Heart attack (also called myocardial infarction) — This happens when the flow of coronary arterial blood to a section of heart muscle is blocked. The affected area of heart muscle begins to die. Cardiovascular (heart and blood vessel) disease over time can lead to a heart attack.
- Sudden cardiac death — This is another term for sudden cardiac arrest. Sudden cardiac death is caused by abnormal heart beats, called arrhythmias. CAD is a leading cause of this condition. Eighty percent of sudden cardiac death cases are linked with CAD. A previous heart attack also puts you at risk for sudden cardiac death. (6)
Signs and Symptoms
Ischemic heart disease grows more serious the longer the blockage in your coronary arteries grows. The blockage in arteries is also known as atherosclerosis. See a doctor right away if you have any of these general symptoms that might affect heart function:
- Shortness of breath — As the blockage in your coronary arteries grows larger, your heart muscle doesn’t pump as well. If your heart isn’t pumping enough to supply your body with healthy, oxygen-rich blood, you may have trouble breathing well.
- Pain in your chest — also called angina. The pain or discomfort in your chest is usually on the left or middle side of your chest or sometimes in the shoulder. The pain also can come when you are in physical or emotional distress. Women especially may feel pain in their jaw, neck, arm or back. (1)
- Angina may be confused with dyspepsia (indigestion) or heartburn.
Angina Symptoms
Additional symptoms of angina include: (3)
- Heavy feeling in the chest
- Feeling of pressure
- Aching
- Burning
- Full feeling in the chest
- Extreme fatigue after exercise or other intense activity (for example, carrying heavy boxes while you are moving). You may get very tired when you do physical activities, because your heart is not pumping enough oxygen-rich blood as it used to.
- Weakness — You may feel weak or numb in your arm or shoulder area or in other ways.
- Dizziness — You may feel unable to stand in a stable position.
- Nausea and vomiting — Nausea and vomiting may be related to heart muscle pain.
Heart Attack Symptoms
Symptoms of heart disease can continue to damage your heart. If a coronary artery becomes completely blocked, this may cause a heart attack. Heart attack symptoms may include: (7)
- Pain in your shoulder or arm
- Heavy, crushing pressure and pain in your chest
- Pain in your jaw or neck
- Pain in your back or stomach
- Shortness of breath
- Sweating
- Cold sweat
- Nausea
- Lightheadedness
Women may have different signs than men have, such as back pain or jaw pain, shortness of breath, or nausea and vomiting.
Causes
Coronary artery disease prevention is possible. You can reduce your risk of disease with natural remedies as well as conventional treatment.
The following are some of the most common coronary artery disease causes: (1)
- High cholesterol — Cholesterol is a form of fat that comes in two varieties: high-density lipoprotein (HDL, known as good cholesterol — you want more of this) and low-density lipoprotein (LDL, bad cholesterol), the type that causes plaque to build up in your arteries. If you have high LDL cholesterol, there are natural remedies to treat the condition.
- High blood pressure — High blood pressure (hypertension) against your blood vessels could cause damage to your arteries and lead to heart attack, heart failure and other serious conditions. It is known as the silent killer because you may not feel worse as the condition develops.
- Diabetes or insulin resistance — Diabetes results in high levels of sugar (glucose) in the blood. Insulin resistance also causes this, but is not as serious as diabetes. Insulin resistance comes before diabetes, and is known as prediabetes. The beta cells in the pancreas cannot produce enough insulin and glucose (sugar) levels begin to rise higher than normal.
- Sedentary lifestyle — Too much sitting and not enough exercise can negatively impact heart health.
- Smoking — Cigarette smoking can damage your blood vessels, increasing the risk of atherosclerosis.
Risk Factors
You can control some CAD risk factors by making lifestyle changes. The following are some of the most common coronary artery disease risk factors: (8)
- Being male — Men have a higher risk of coronary artery disease. Risk for women rises after they go through menopause.
- Family history — Some people may have heart disease with genetic origins. Sudden cardiac death data show a link between genetics and the risk of dying suddenly, but more research is needed. Uncovering arrhythmia risk (irregular heartbeats) is a better use for genetic testing at this time. It may help to look back a couple of generations and see if there are patterns of heart disease in your family, in addition to knowing your own risk factors. (9)
- Age — Hearts and blood vessels work less well over time.
- Smoking
- High stress levels
- Physical inactivity
- Being overweight or obese
- Inflammation in your body — Some inflammation markers play a key role in development of atherosclerosis. (10)
- Sleep apnea — Sleep apnea (uncontrollable pauses in your breathing while sleeping) is common in CAD patients. This apnea may be linked with chronic inflammation, which may be linked to CAD getting worse or other conditions involving the vessel around the heart. (11)
- Diabetes
- End-stage renal disease — If your kidneys are in advanced stages of kidney (renal) disease, you may have faster plaque buildup in your arteries. A study showed that more than half of dialysis patients in Western Europe and North America had a premature death because of cardiovascular disease. (12)
- High blood pressure — This condition puts more pressure against artery walls, which over time can damage the arteries.
- High blood cholesterol — Too much LDL cholesterol leads to buildup of plaque.
- Metabolic syndrome — People with metabolic syndrome have a number of combined factors that leave them open to more diseases states, like coronary artery disease. One study showed that high cholesterol, obesity in the center of the body and high blood sugar together were more common risk factors for CAD. (13)
Conventional Treatment
Coronary artery disease treatment often includes lifestyle changes, and there are also drugs for some of the symptoms and conditions you may have.
You may not be able to reverse all of the plaque that builds up in your arteries, but you can prevent more buildup and slightly reduce the level of plaque you have. Even if your doctor prescribes a statin drug to lower cholesterol, you’ll still need to eat healthy foods and stay physically active. (14)
Once you have a coronary artery disease diagnosis, you may wish to discuss your particular coronary artery disease pathophysiology (what processes in your body led to CAD). Talk to a medical professional about whether you should take drugs, including: (15)
- Drugs that lower cholesterol. Some drugs reduce the amount of LDL cholesterol in your blood and thus reduce the amount of plaque in your coronary arteries. These drugs include niacin, statin drugs, fibric-acid drugs to reduce triglyceride fats and bile acid sequestrants.
- Aspirin. Your doctor may recommend taking a daily aspirin or other drugs that can thin your blood.
- Angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARBs). These drugs decrease blood pressure and may help prevent progression of coronary artery disease.
- Beta blockers. These drugs slow your heart rate and decrease your blood pressure, which reduces the need for oxygen. Beta blockers reduce the risk of future heart attacks, if you have already had one.
- Nitroglycerin. Nitroglycerin tablets, sprays and patches can manage chest pain by opening up (dilating) your coronary arteries for short periods of time.
How to Help You Recover from CAD Naturally
There are many natural ways you can get relief for your case of CAD. Coronary artery disease treatment includes several natural remedies that you can try:
1. Eat your way to better heart health
Because LDL cholesterol (bad cholesterol) levels affect your health, you should add foods into your diet that are low in cholesterol. Foods high in soluble fiber also are a great addition to your diet. You should avoid saturated or hydrogenated fats, because saturated fats can turn into cholesterol. Here are some foods to add and some you should avoid for coronary artery health. These foods are also good for you if you have diabetes. (16, 17)
Add:
- Whole grains, whole-grain breads and cereals
- Navy beans, kidney beans, chick peas
- Fat-free or 1 percent milk
- Raw or cooked fruits with low-fat yogurt
- Fish
- Garlic as a cooking ingredient
- Moderate amounts of nuts
- Olive oil in small amounts when you cook
Avoid:
- Large amounts of oils, especially corn and peanut oils
- Fried foods, like potato chips, French fries and other junk foods
- Butter and margarine
- Egg yolks
- Whole milk or cream
- Foods cooked in butter, cheese or cream (including vegetables)
- Bacon, sausage and organ meats, like liver
- Sugary desserts and candy; eat smaller portions of dessert.
2. Lower cholesterol with exercise
Exercise of all kinds can help you lower LDL cholesterol. It also helps prevent plaque buildup and raise HDL (good) cholesterol. Being active also helps by improving other atherosclerotic risk factors such as high blood pressure, diabetes, obesity, stress and various other factors that promote blood clots. Check with your doctor before you start an exercise program to make sure your heart and other systems are ready.
Exercise that raises your heart rate and makes you breathe harder (aerobic exercise) is very helpful. Examples include: (18)
- Walking — this is at the top of many lists for exercise that benefits your cardiovascular system. Walk two to three miles any day that you can.
- Light jogging
- Biking
- Swimming
Here are some tips for making your exercise program more of a joy and a success:
- Make sure you pick an exercise you really enjoy
- Exercise to music
- Exercise with a buddy who is at your level of activity
- Commit by planning how and when you will exercise. You may not feel like it, but if you have made the choice, exercise a little anyway.
- You can build more activity into your day by taking breaks from your desk and walking, stretching or doing yoga, or dancing.
3. Lose weight
In several studies, a defined weight loss program was linked to improved outcomes for patients with coronary artery disease. In one study, a low-calorie diet and an exercise program were equal in terms of helping patients increase their cardiac blood flow. (19)
With a healthy combination of diet and exercise tips above, you should begin to lose weight, which can take some of the burden off of your coronary arteries. Talk to your doctor anytime you start a new diet or exercise program.

4. Manage stress
Stress can damage your heart. If you are often under stress, you will more likely have heart disease, high blood pressure, chest pain or irregular heartbeats. Stress can raise your blood pressure to unhealthy levels. (20) Several studies have also shown the effects of chronic stress as it relates to the inflammation aspect of atherosclerosis. (21)
Thankfully, studies have shown that regular programs of mindfulness-based stress reduction and of meditation to reduce stress have improved the health of patients with atherosclerosis. (22) Stress reduction of other kinds may help you relax as well.
Healthy habits can come to your rescue in times of stress:
- Working out
- Saying no to caffeine
- Saying no to alcohol
- Getting a good night’s sleep
- Meditating or praying
- Spending time with friends, family or pets.
5. Stop smoking
The chemicals in tobacco smoke harm your blood cells. They also can damage the function of your heart and the structure and function of your blood vessels. This damage increases your risk of atherosclerosis, another name for the build-up of plaque in your arteries. (23)
You might try natural approaches to help quit smoking: (24)
- Yoga
- Exercise
- Mindfulness meditation
- Hypnosis
- Tai chi
- Writing down a quit plan
6. Try aromatherapy
Evidence shows that aromatherapy can lower your levels of stress and anxiety, and some evidence even shows that you can affect your cardiovascular system with aromatherapy as well. A 2012 study found that aromatherapy using essential oils can lower blood pressure through relaxation. Only short periods of breathing in an essential oil was helpful. According to the same study, smelling oils for more than an hour might be harmful. (25)
If you’d like to try using essential oils to lower your heart disease risk, these are some of your best bets: (26)
- Basil — Extract from basil leaves shows potential for lowering levels of LDL cholesterol, as demonstrated in a recent animal study. (27)
- Cassia — Research from another animal study shows that cassia flower extract reduces blood glucose levels while increasing insulin. (28)
- Clary sage — Research from Korea shows that oil vapors from the white-pink flowers of this wide-leafed shrub are effective at decreasing systolic blood pressure (the top number in a blood pressure reading). (29)
- Cypress — Cypress oil used in aromatherapy massage provides short-term relaxation and relief from fatigue. (30)
- Lavender — Research on lavender oil found that it produces an overall calm and relaxed mood when inhaled. (31)
- Marjoram — When inhaled, the oil from this herb lowers blood pressure. (32)
7. Consider taking glucosamine
A study published in May, 2019 in the BMJ found evidence that habitual use of glucosamine supplements, which are commonly taken to help relieve osteoarthritis pain, may also be related to lower risks of cardiovascular disease (CVD) events. (33) In this large prospective study, habitual glucosamine use was associated with a 15 percent lower risk of total CVD events and a 9 to 22 percent lower risk of individual cardiovascular events. The protective effects of glucosamine on CVD outcomes were even stronger among current smokers.
The study followed over 466,000 participants without heart disease at the beginning of the study from 2006 to 2010 and tracked their supplement use. Researchers then followed up with the participants again in 2016. It was found that after adjusting for age, sex, body mass index, race, lifestyle factors, dietary intakes, drug use, and other supplement use, glucosamine use was associated with a significantly lower risk of total CVD events, CVD death, coronary heart disease development and stroke.
Glucosamine is a crystalline compound which is found inside connective tissue and cartilage. It’s made from chains of sugars and proteins bound together. It’s estimated that approximately 20 percent of adults living in the U.S and Australia consume glucosamine supplements daily, since this popular supplement is available over-the-counter in these countries and known to help with joint pain. Emerging evidence has linked use of glucosamine with not only reduced joint pain and now prevention of cardiovascular disease/atherosclerosis, but also reduced mortality, reduced inflammation, and extended life span (according to some animal studies).
How may glucosamine help protect the heart and arteries? Evidence from the National Health and Nutrition Examination Survey (NHANES) study found that glucosamine was associated with a statistically significant reduction in C reactive protein concentrations, which means it can help lower systemic inflammation, thereby playing a preventive role in the pathophysiology of CVD. Glucosamine also seems to mimic the protective effects of a low-carbohydrate diet, since it can decrease glycolysis (the breakdown of glucose by enzymes) and increase breakdown of proteins.
Precautions
There are many ways you can protect yourself from coronary artery disease and its symptoms and complications:
- Go to your doctor with pain, shortness of breath or severe heart symptoms. Don’t wait for severe chest pain to go away — the complications of CAD can be deadly.
- Learn your family heart history as soon as you can, especially if there is sudden cardiac death among your relatives.
- Get tested for your cholesterol levels, and do what you can to lower LDL cholesterol with natural remedies or with medications; be sure to do so under physician supervision.
- Get tested for prediabetes and diabetes. Know your glucose levels. Eating the right foods can help you lower blood sugar.
- See a medical professional before you start a new diet or exercise program.
- Stop smoking if at all possible and reduce the amount of alcohol you drink.
Final Thoughts
- Coronary artery disease can lead to heart disease and heart attacks.
- Serious heart disease can be a quiet attacker or can show up with a lot of different symptoms. Learn the most common symptoms of heart disease related to CAD and don’t ignore them.
- CAD is more common in men, older people, people with diabetes and smokers.
- Diet and exercise make a difference in your artery health.
- Avoiding stress, finding ways to calm yourself and getting better sleep are also ways to help you manage CAD.
6 Natural Ways to Help Beat Coronary Artery Disease
- Eat your way to better heart health
- Lower cholesterol with exercise
- Lose weight
- Manage stress
- Stop smoking
- Try aromatherapy
Read Next: These 5 Heart Disease Tests Could Save Your Life (And Your Doctor Probably Isn’t Ordering Them)








