This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Natural Approach to Managing Manic Depression (Bipolar Disorder)
April 14, 2016

Do you or someone you know experience extreme mood swings with any type of recurring frequency? I’m talking about things like manic “high” period of increased energy in rotation with very “low” periods of depression. If so, it may a sign of manic depression.
Although many people live with manic depression, also known as bipolar disorder, many are never accurately diagnosed. Experts believe at least 5 million to 6 million people suffer from this condition in the U.S. alone.
While even healthy people experience many changes in their moods throughout the day and over the course of their lifetimes, those with manic depression are prone to much more abrupt and drastic “ups and downs.” The majority of people with manic depression experience so much low (depression) and high (manic) phases that their quality of life is significantly impaired. This greatly affects their ability to live normally, hold relationships, take care of their bodies, work and communicate with others.
Bipolar disorder impacts just about every facet of someone’s life, including that person’s thoughts, bodily sensations, sleep, personality and behaviors. During the high manic periods of manic depression, symptoms usually include restlessness, rage, hallucinations and aggression. On the other hand, during the low episodes symptoms are those common to depression, such as fatigue, despair, loss of motivation and social isolation. Although the exact cause of manic depression isn’t entirely known, some of the factors contributing to its development include genetics, brain chemistry, childhood environment and life events.
Like clinical/major depression and other mental disorders, manic depression is a condition that needs to be controlled carefully throughout someone’s lifetime. Becoming educated on the condition and its early warning signs, getting professional help, and reducing anxiety and depression through a healthy lifestyle and lowering stress can all help manage manic depression. Finding out all you can about how bipolar disorder develops, progresses and is sustained can help you or a family member deal with the symptoms of this sometimes-debilitating condition.
Natural Treatments to Help Manic Depression
Bipolar disorder can be progressive and worsen over time when left undiagnosed. Some people wind up having more drastic mood swings/episodes, and more frequently, as time goes on and symptoms are not treated. Although it cannot be cured entirely in most cases, managing symptoms can prevent frequent mood swings and suicidal, destructive behaviors.
Just like with clinical depression or anxiety, many doctors choose to control bipolar disorder using medications (such as mood stabilizers, antipsychotics, antidepressants and anti-anxiety drugs). (1) However, there are many effective natural treatments that can also help control symptoms of manic or depressive phases, and these have practically zero negative side effects, unlike psychotropic drugs.
Treatment for depression and bipolar disorder has come a long way, and today many individuals are able to receive help that significantly improves their quality of life, relationships, levels of independence and ability to live happy lives. Even when medication is used, these treatment options below can help stabilize the condition and improve recovery.
1. Education and Medical Care
Many experts feel that becoming educated about manic depression — learning about its symptoms and adopting a plan to recognize the early warning signs of a depressive or manic episode — can be one of the best tools. This helps develop problem-solving skills and establishes a plan for what to do when depression or mania starts emerging, such as telling a family member/friend or speaking with a therapist as quickly as possible. Meeting others with bipolar depression, reading online about helpful tips, and enhancing your life with things like physical activity, meditation and creative projects can boost self-esteem and keep up a more peaceful environment.
Cognitive behavioral therapy (CBT) is one type of therapy that has shown promise for naturally managing bipolar disorder episodes. CBT can help you start to recognize underlying thought patterns that trigger mood swings; be attentive to your feelings, body sensations and emotions before they turn into more severe symptoms; and help you to learn to reach out for help when you notice you’re in a difficult frame of mind (such as experiencing more anxiety or losing sleep).
In one Systematic Treatment Enhancement Program for Bipolar Disorder study, researchers compared people in two groups — those undergoing collaborative care therapy versus intensive CBT psychotherapy — over nine months and found those practicing CBT had fewer relapses, lower hospitalization rates and were better able to stick with their treatment plans even one year later. (2)
No matter the type of therapy approach you choose, some of the ways to help improve your therapy sessions and recovery include:
- being open and honest
- gaining support from your family (even including them in therapy sessions)
- creating a daily planner to help manage stress and stay organized
- keeping a journal of your feelings
- staying open-minded to suggestions from your therapist
- taking care of yourself in other ways between therapy sessions that can increase happiness (like eating right and getting enough sleep)
- joining a support group or group therapy class is another great way to lower stress about manic depression, connect with other people going through the same thing and receive valuable advice from others who have recovered. Many support groups exist around the U.S., are easy and free to join, and can be found on the Depression and Bipolar Support Alliance website.
2. Exercise (Ideally Outdoors)
Exercise is practically a natural depression remedy since it’s a helpful way to lower stress, build confidence, help with getting good sleep, take care of your body, and even connect with other people if you a join a group team or cause. Many therapists who work with patients with depression or anxiety recommend taking a walk outdoors every day, regardless of the weather or time of year, to stay in touch with nature, the seasons and the elements around you.
Exercising outdoors has all the same benefits of exercising inside (it’s good for your heart, immunity, bones and weight, for example), plus it exposes you to uplifting natural light, connects you to what’s going on around you and tends to make you “see the bigger picture” more easily. These help lower anxiety, feelings of isolation, fatigue and hopelessness.
This is supported by research. A 2016 study published in the Journal of Affective Disorders found that “exercise was associated with improved health measures including depressive symptoms, functioning and quality of life.” (3)
3. Eating a Healthy Diet
You might be surprised to know how much altering your diet can change how you feel. Some studies have found that those who eat diets high in processed and fast foods are up to 60 percent more likely to suffer from depression compared to people eating healthier diets. (4) Your diet can greatly affect hormone production, neurotransmitter functions, energy and other processes that influence your overall mood.
As part of an anti-depression diet, it’s best to avoid foods that have lots of sugar, added sodium and artificial ingredients, in addition to greatly cutting back or eliminating caffeine and alcohol. Some of the best foods for fighting anxiety and depression include:
- Healthy fats — coconut, raw dairy and grass-fed meats (saturated fat supports cellular function and neurological health)
- Clean, lean protein foods — cage-free eggs, wild fish, grass-fed meat and pasture-raised poultry. Try to have at least four to five ounces of high-quality lean protein at every meal to get a variety amino acids that are important for hormonal balance
- Wild-caught fish — omega-3 fatty acids found in fish like salmon, halibut, sardines and mackerel are critical to maintain a healthy brain
- Vegetables and fruit — increase your intake of vital nutrients and antioxidants that support mood
- High-fiber foods — nuts and seeds, such as flax, chia, hemp and pumpkin seeds, provide essential fiber in addition to omega-3s for brain function and fiber. Fiber is also found in fresh produce, ancient grains and beans/legumes
There are even some case studies that suggest the keto diet could positively impact symptoms of manic depression. Two patients following the diet to remain in a state of ketosis (achieved by drastic carbohydrate reduction and high fat intake) were observed for multiple years. Both reported a stabilization of mood while on the diet they claimed exceeded their medication and resulted in little to no side effects. (5)
Related: How Dialectical Behavior Therapy (DBT) Works + Benefits
4. Yoga and Meditation
Mindfulness meditation is similar to CBT, as it’s an effective way to recognize when your mood is becoming problematic, you’re getting stuck in ruminating thought patterns, and external situations are causing you to feel stressed, angry or vulnerable. Meditation (and similarly, even healing prayer) practices can be done entirely on your own time at home, are free, simple and have been trusted for improving emotional control for thousands of years. Yoga, considered a form of “moving meditation,” is also beneficial for the same reasons and is suitable for people who find it hard to meditate sitting or laying still.
A 2011 study published in the Journal of Psychiatric Practice found that people with bipolar disorder who participated in a mindfulness-based cognitive therapy program for eight weeks reported significant improvements in executive functioning, memory, and ability to initiate and complete tasks, as measured by the Behavior Rating Inventory of Executive Function and the Frontal Systems Behavior Scale. They also experienced “changes in cognitive functioning which were correlated with increases in mindful, nonjudgmental observance and awareness of thoughts, feelings, and sensations, and were not associated with decreases in depression.” (6)
5. Herbs and Supplements
Certain herbs and supplements have been shown to improve depressive symptoms and can help control anxiety. (7) These include:
- Natural plant-based adaptogens herbs, including gingeng, holy basil, ashwaganda and rhodiola, help control the body’s stress response, lower cortisol, improve energy/focus and balance hormones in various ways.
- St. John’s wort (Hypericum perforatum) is a natural antidepressant that can be helpful for getting good sleep.
- Omega-3 fatty acids are derived from fish oil and help lower depression symptoms and inflammation.
- Essential oils for depression include lavender, bergamot, ylang ylang and chamomile, which can be used in the shower, inhaled/used for aromatherapy, or applied to the skin as a way of bringing on relaxation and reducing muscle tension.
- When people with manic depression add a high-quality probiotic supplement to their routine, the rate of rehospitalization from manic episodes goes down significantly. (8) That’s not surprising, considering the gut-brain connection that greatly influences mental health.
6. Reducing Stress
Any activity or hobby that feels fun, reaffirming, creative and soothing is a good way to blow off steam and control depressive or manic symptoms in a skillful, positive way. Different things work for different people to help relieve stress, including keeping a journal or writing, doing art or listening to music, spending time outdoors, taking a relaxing bath, or spending more time with family and friends. It’s important to cut out time every day to specifically do things that make you feel connected to others, happy and relaxed, even if it’s just for a short period of time (such as one hour at night before bed or first thing in the morning).
The more that you can make stress-reducing activities part of your regular routine, the likelier you are to stick with them and manage your symptoms. (9) It helps to make plans for fun, social activities that you can look forward to in the future and to keep organized in terms of keeping up with therapy appointments.
One helpful practice is keeping a journal in which you record how you’re feeling each day in order to track symptoms and draw some patterns. You can try recording your thoughts, feeling and behaviors daily in order to see what kind of activities keep you feeling most stable and happy, compared to those that make you feel vulnerable and easily triggered into experiencing mood swings.
Facts About Manic Depression
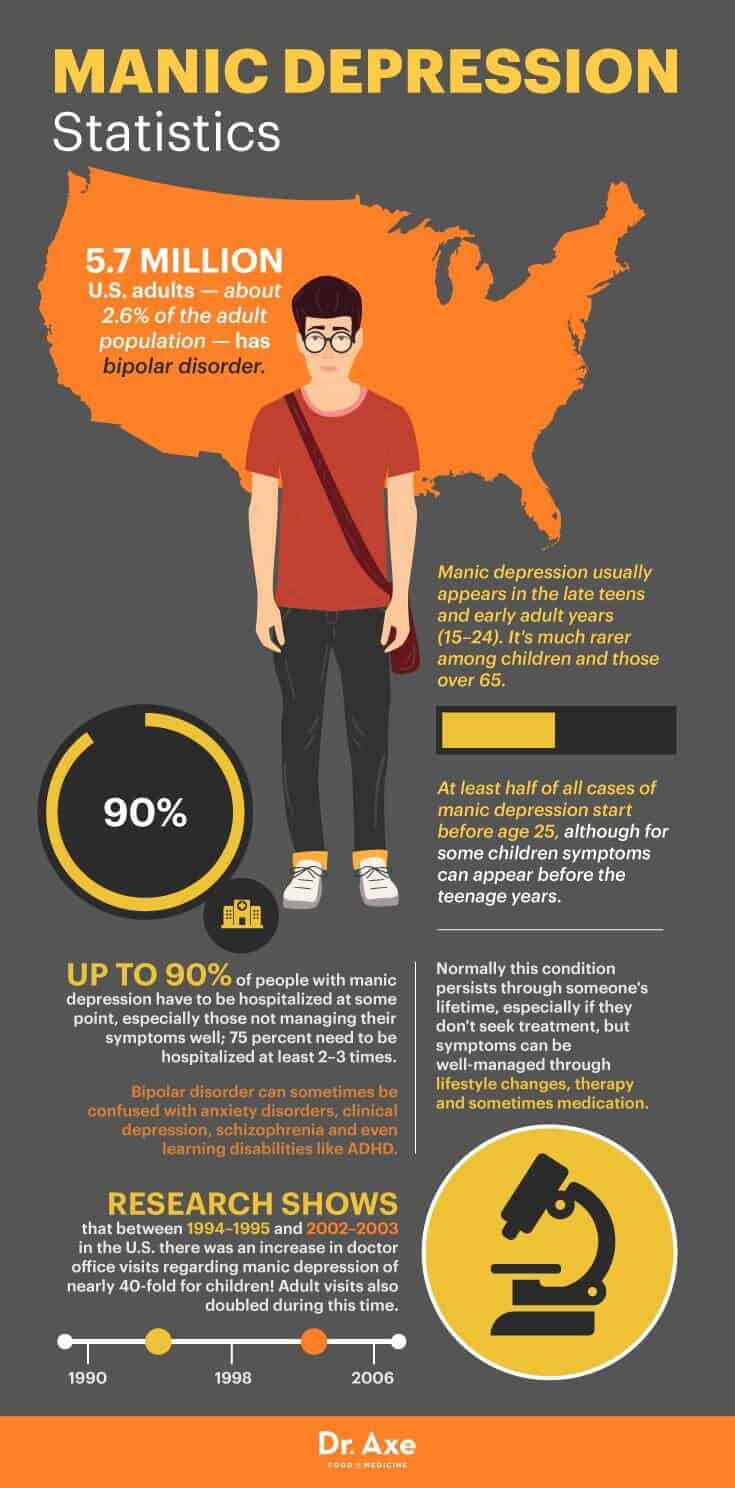
- 5.7 million American adults (about 2.6 percent of the U.S. population 18 and older) have bipolar disorder, according to the National Institute of Mental Health. (10)
- Manic depression/bipolar disorder usually appears in the late teens and early adult years (especially between ages 15 and 24). It’s much rarer among children and those over 65 years old.
- At least half of all cases of manic depression start before age 25, although for some children symptoms can appear before the teenage years.
- Normally this condition persists through someone’s lifetime, especially if the person doesn’t seek treatment, but symptoms can be well-managed through lifestyle changes, therapy and sometimes medication.
- Up to 90 percent of people with manic depression have to be hospitalized at some point, especially those not managing their symptoms well; 75 percent need to be hospitalized at least two to three times. (11)
- Bipolar disorder can sometimes be confused with anxiety disorders, clinical depression, schizophrenia and even learning disabilities like ADHD (especially in children and teens, who can display hyperactive behaviors similar to mania). (12)
- Research shows that between 1994–1995 and 2002–2003 in the U.S., there was an increase in doctor office visits regarding manic depression of nearly 40-fold for children! Adult visits also doubled during this time.
Depression vs. Manic Depression
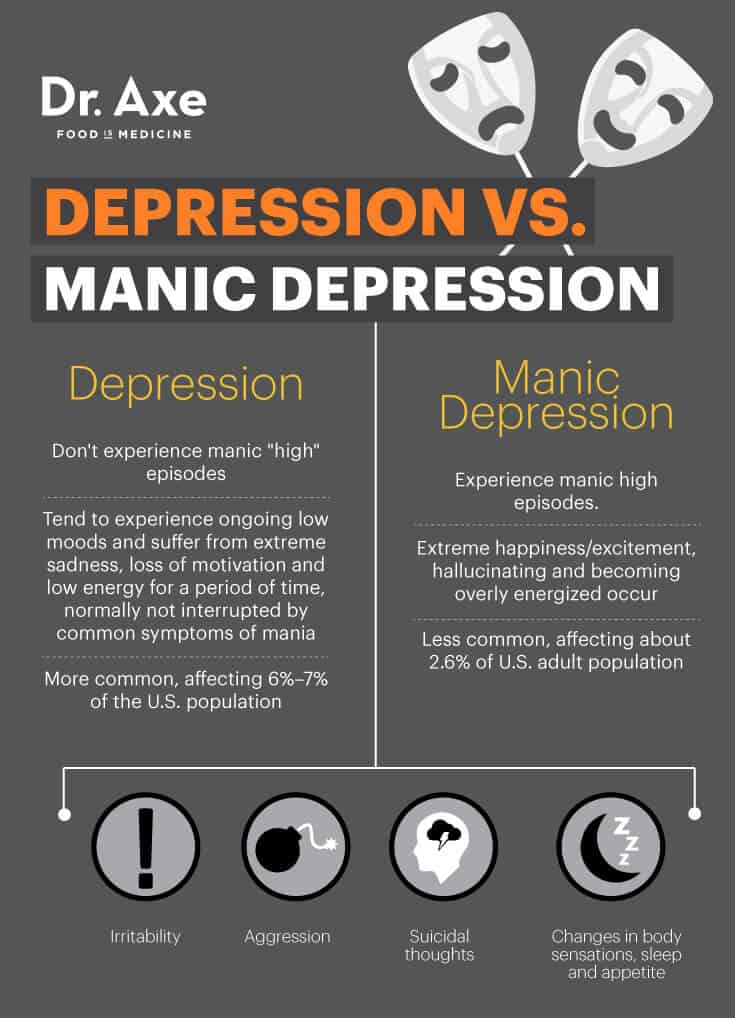
The primary difference between depression (whether clinical, short-term or major depression) and manic depression is that people with depression don’t experience manic “high” episodes. Those with depression tend to experience ongoing low moods and suffer from extreme sadness, loss of motivation and low energy for a period of time, normally not interrupted by common symptoms of mania like extreme happiness/excitement, hallucinating and becoming overly energized, for example. Depression is also more common than manic depression, affecting about 6 percent to 7 percent of the U.S. population at any given time. (13)
Although they have important differences, bipolar disorder/manic depression and clinical depression do have some similarities. They can both cause irritability, aggression, suicidal thoughts, and changes in body sensations, sleep and appetite.
A lesser form of mania, called hypomania (also referred to as bipolar disorder II), can also accompany some people with depression. Compared with bipolar disorder/manic depression, those with hypomania usually experience much less severe and life-impairing manic symptoms.
According to the DSM-5, the diagnostic manual published by the American Psychiatric Association that helps psychiatrists diagnose mental disorders, those with hypomania also have an absence of psychosis (delusions or hallucinations), and their work, relationships and general quality of life don’t suffer from manic symptoms. (14)
Symptoms of Manic Depression (Bipolar Disorder)
Throughout a given time period, those with bipolar disorder experience very different symptoms, depending on whether they are currently in a manic phase or on the other side of the pendulum in a depressive phase. Symptoms and moods also differ a lot from person to person. For most people, either very high or very low moods are experienced for several days at a time. Others might stay in a manic or depressive phase for several months.
Most people with bipolar disorder have stable, normal moods with few symptoms for stretches of time, but on the other hand some hardly ever feel “normal” and jump from one end of the spectrum to the other over and over again.
Common manic symptoms include:
- very happy moods and excitement
- hallucinations/psychosis or delusions (seeing and hearing things that don’t actually exist, sometimes thought of as “increased creativity”)
- at times paranoia and extreme anxiety
- irritability, aggression and sometimes rage
- insomnia and trouble sleeping normally
- strong motivation and ideas related to new plans
- loss of appetite and sometimes weight loss
- fast talking and fidgeting
- spending more money than usual on affordable things or spending lots of energy/time on unnecessary projects
Common depression signs and symptoms include:
- very low moods, including feeling worthless, insignificant and hopeless
- for some suicidal thoughts can occur
- fatigue or lethargy (even though many people tend to sleep for long duration during this phase)
- low motivation
- brain fog and trouble concentrating, working, making decisions and remembering things
- loss of interest or enjoyment in activities and hobbies
- higher likelihood for abusing alcohol and drugs
Many times someone with manic depression will seek medical help and receive a diagnosis when that person has been in a depression phase for some time. This might be when family, co-workers and friends are more likely to notice a change in personality and suggest seeking treatment. On the other hand, many people with bipolar disorder never choose to get help and therefore continue to suffer unnecessarily. Seeking help from a therapist can be on the most important thing someone with manic depression does, since research shows that up to 20 percent of people who leave depression or other mood disorders untreated wind up taking their own lives. (15)
Causes of Bipolar Disorder/Manic Depression
- Genetics: Like depression, anxiety and other mental disorders, there’s a genetic component to bipolar disorder, and it tends to run in families. According to the National Institute of Mental health, people with certain genes are more likely to develop bipolar disorder than others, although genetics alone are not likely to cause the condition. Even identical twins who have bipolar disorder in their family don’t always have the same outcome despite having identical genes. Most children with a family history of bipolar disorder will not develop the illness, and it seems that other factors need to trigger its development, including life events, upbringing and lifestyle habits that affect the brain.
- Chemical imbalances and brain functioning: The brain’s physical structure and chemical activities affect someone’s moods and are related to the onset of mental disorders, including manic depression. Some research has shown that brains of people with bipolar disorder are different from those of healthy people, sometimes showing “multi-dimensional impairments” that are similar to those seen in people with schizophrenia (another disorder that features mood swings). It’s possible that ongoing inflammation also worsens these structural and chemical changes.
- Lifestyle/upbringing: Research using MRI brain scans has found that the part of the brain called the prefrontal cortex (associated with “executive” functions, such as solving problems and making decisions) in people with bipolar disorder tends to be smaller and less active compared to adults who don’t have bipolar disorder. Psychiatric experts still have a lot to learn about how different upbringings and environments change brain structures, but it seems that someone’s recurring negative/fearful thoughts and behaviors can actually physically change the brain’s chemical channels through “neuroplasticity.” This increases the odds of experiencing harmful moods more often in the future and developing mood-related disorders. (16)
Key Points about Manic Depression (Bipolar Disorder)
- Experts believe at least 5 million to 6 million people suffer from this condition in the U.S. alone.
- Manic depression/bipolar disorder usually appears in the late teens and early adult years (especially between ages 15 and 24). It’s much rarer among children and those over 65 years old.
- Up to 90 percent of people with manic depression have to be hospitalized at some point, especially those not managing their symptoms well; 75 percent need to be hospitalized at least two to three times.
- Even when medication is used, these treatment options below can help stabilize the condition and improve recovery: education and medical care, exercise ideally outside, eating a healthy diet, yoga and meditation, certain herbs and supplements, and reducing stress.
- Common manic symptoms include very happy moods and excitement; hallucinations/psychosis or delusions; at times paranoia and extreme anxiety; irritability, aggression and sometimes rage; insomnia and trouble sleeping normally; strong motivation and ideas related to new plans; loss of appetite and sometimes weight loss; fast talking and fidgeting; spending more money than usual on affordable things or spending lots of energy/time on unnecessary projects. Common depression signs and symptoms include very low moods, including feeling worthless, insignificant and hopeless; suicidal thoughts; fatigue or lethargy; low motivation; brain fog and trouble concentrating, working, making decisions and remembering things; loss of interest or enjoyment in activities and hobbies; higher likelihood for abusing alcohol and drugs.
- The three main causes of manic depression seem to be genetics, chemical imbalances and brain functioning, and lifestyle/upbringing.
- The primary difference between depression (whether clinical, short-term or major depression) and manic depression is that people with depression don’t experience manic “high” episodes. Those with depression tend to experience ongoing low moods and suffer from extreme sadness, loss of motivation and low energy for a period of time, normally not interrupted by common symptoms of mania like extreme happiness/excitement, hallucinating and becoming overly energized, for example. Depression is also more common than manic depression, affecting about 6 percent to 7 percent of the U.S. population at any given time.








