This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Symptoms of Schizophrenia (+ 7 Natural Ways to Help Schizophrenia Treatment)
June 28, 2018

Of the psychiatric diagnoses in our modern world, schizophrenia holds a particularly infamous position. The symptoms of schizophrenia are thought by many to be debilitating, incurable and even scary. It’s no wonder, considering the way schizophrenia is portrayed in entertainment — most of us have seen at least one episode or movie in which a schizophrenic patient is portrayed as the crazy, violent antagonist.
However, while this mental illness is definitely serious, there are many ways to manage symptoms of schizophrenia, both in conventional treatment methods and by natural means. Let’s take a look at a basic overview of schizophrenia: what it is, why it may happen to some people, how it’s typically treated and natural ways to manage schizophrenia symptoms.
What Is Schizophrenia?
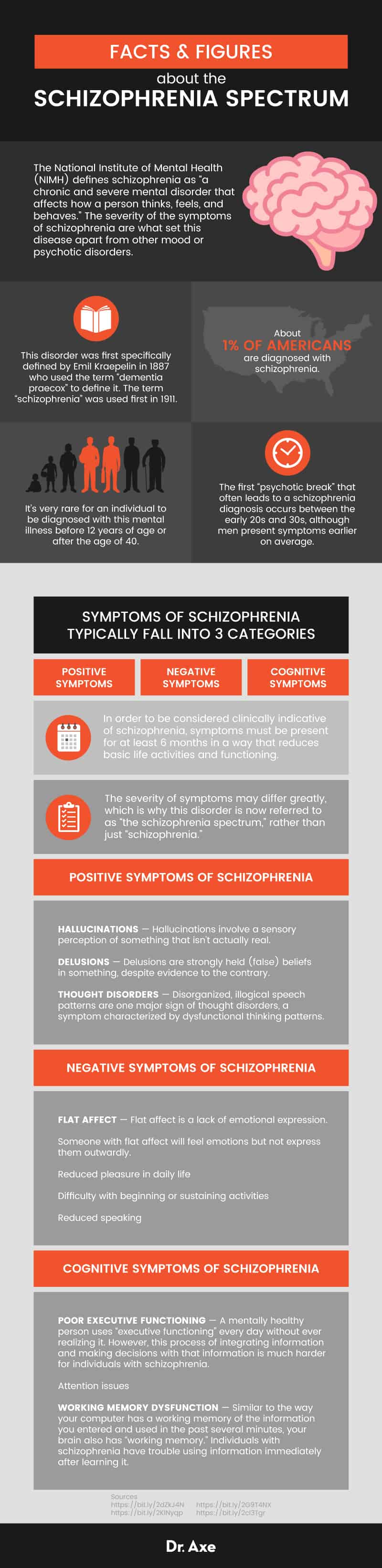
The National Institute of Mental Health (NIMH) defines schizophrenia as “a chronic and severe mental disorder that affects how a person thinks, feels, and behaves.” (1) The severity of the symptoms of schizophrenia are what set this disease apart from other mood or psychotic disorders.
This disorder was first specifically defined by Emil Kraepelin in 1887 who used the term “dementia praecox” to define it. The term “schizophrenia” (meaning split, or fragmented, mind) was used first in 1911. Other outdated terminology for disorders resembling schizophrenia include melancholy; folie circulaire; hebephrenia; a silly, undisciplined mind; and catatonia. (2)
According to the National Alliance on Mental Illness (NAMI), about 1 percent of Americans are diagnosed with schizophrenia. Technically, it can occur and be diagnosed at any age, but the first “psychotic break” that often leads to a schizophrenia diagnosis occurs between the early 20s and 30s, although men present symptoms earlier on average. It’s incredibly rare for an individual to be diagnosed with this mental illness before 12 years of age or after the age of 40. (3)
The best news is that it is possible to have a healthy and fulfilling life despite this stigmatized diagnosis. For example, one Cochrane review found that supported employment (offering support and training on-the-job tailored to the individual’s needs) is a somewhat effective method of helping a schizophrenic person maintain a job. (4) One key here is that individuals with schizophrenia need a support system around them willing to aid them in recovery and look past the public assumptions about the diagnosis.
Signs and Symptoms
Symptoms of schizophrenia typically fall into three categories: positive symptoms, negative symptoms and cognitive symptoms. “Positive” symptoms are outwardly eccentric, “negative” symptoms of schizophrenia are internally depressive and “cognitive” symptoms impact basic brain and memory functions.
While the positive symptoms are the most well-known in many cases, negative and cognitive symptoms must also be present for a diagnosis. During the “prodromal” period (before positive symptoms manifest), teenagers with schizophrenia may be diagnosed with depression, since negative symptoms often mimic traditional depression. But how is schizophrenia diagnosed?
In order to be considered clinically indicative of schizophrenia, symptoms must be present for at least six months in a way that reduces basic life activities and functioning. In addition, the DSM-V calls for “at least one month of active-phase symptoms,” which include delusions, hallucinations, disorganized speech, disorganized or catatonic behavior and negative symptoms. The severity of symptoms may differ greatly, which is why this disorder is now referred to as “the schizophrenia spectrum,” rather than just “schizophrenia.” (5)
Some of the symptoms of schizophrenia include: (1)
Positive Symptoms of Schizophrenia
- Hallucinations — Hallucinations involve a sensory perception of something that isn’t actually real.
- Delusions — While these are often confused with hallucinations, delusions are strongly held (false) beliefs in something, despite evidence to the contrary. This symptom is also present in obsessive-compulsive disorder.
- Thought disorders — Disorganized, illogical speech patterns are one major sign of thought disorders, a symptom characterized by dysfunctional thinking patterns.
Negative Symptoms of Schizophrenia
- Flat affect — Also recognized as a symptom of traumatic brain injury, autism and depression, flat affect is a lack of emotional expression. Someone with flat affect will feel emotions but not express them outwardly.
- Reduced pleasure in daily life
- Difficulty with beginning or sustaining activities
- Reduced speaking
Cognitive Symptoms of Schizophrenia
- Poor executive functioning — A mentally healthy person uses “executive functioning” every day without ever realizing it. However, this process of integrating information and making decisions with that information is much harder for those with schizophrenia.
- Attention issues
- Working memory dysfunction — Similar to the way your computer has a working memory of the information you entered and used in the past several minutes, your brain also has “working memory.” Peolpe with schizophrenia have trouble using information immediately after learning it.
To diagnose schizophrenia, a qualified medical professional should observe at least two of the following symptoms for a one-month period of time (one of which must be in the first three symptoms listed): (5)
- Delusions
- Hallucinations
- Disorganized speech
- Disorganized or catatonic behavior
- Negative symptoms
Unlike the NIMH and NAMI, the DSM-V criteria define symptoms as falling into only negative and positive symptoms. During the six months prior to diagnosis, the psychiatrist should also see evidence of “prodromal or residual symptoms,” meaning less-outwardly severe negative symptoms before or after active positive symptoms.
Schizophrenia Subtypes
In the past, there were five schizophrenia subtypes: paranoid, disorganized, catatonic, undifferentiated and residual. However, in 2013, the DSM-V made some major changes to the disorder classifications. The most significant change was the removal of all five subtypes of the disorder; while many people still think hallucinating or believing other people are out to harm them are paranoid schizophrenia symptoms, that term is now outdated.
This change was made because clinicians agreed that using these subtypes was not helpful in either identifying or treating this mental illness, nor are they always consistent during the course of the disease. (6)
Causes and Risk Factors
Like all mental illnesses, the schizophrenia spectrum has a combination of causes and risk factors that can only be somewhat defined. However, there are several physiological signs and risk factors associated with schizophrenia. Known causes and/or risk factors for schizophrenia include:
- Multiple gene encoding errors/malfunctions (7, 8)
- Smaller mass of brain matter (particularly for early-onset symptoms) (9)
- Decreased immune system function (10)
- White matter abnormalities in the brain (11)
- Excessive free radical activity (12, 13, 14, 15)
- Celiac disease (16)
- Small gestational size in utero and a mother who bled during pregnancy (17)
- A family member with schizophrenia, especially a mother, father or sibling (18)
- Infection with T. gondii, a parasite that causes toxoplasmosis, sometimes caused by a household cat (19, 18)
- Being born or raised in an urban area (20, 18)
- Use of cannabis (18)
- Autoimmune disease (21)
- Childhood sexual abuse (lower but still significant risk) (18)
- History of traumatic brain injury (lower but still significant risk) (18)
- Birth complications (lower but still significant risk) (18)
Conventional Treatment
Medications
In conventional psychiatry, drugs are the first-line treatment recommended by the DSM. These antipsychotics, also referred to as neuroleptics, are associated with an incredibly large list of severe symptoms and risks (more, in fact, than other classes of psychotropic drugs). For that reason, and sometimes a lack of understanding of their disorder, those prescribed antipsychotics have a significant chance of being “non-compliant,” which means they may stop taking their medication without medical supervision.
Medications for schizophrenia are divided into first generation (typical) and second generation (atypical) antipsychotics. Typical antipsychotics are associated with side effects that involve losing some control over basic movements. These movement disorders, such as dystonia, tardive dyskinesia and akathisia, can be very difficult to live with.
Atypical antipsychotics are generally preferred because they cause less movement disorder problems. However, they are associated with other side effects including major weight gain and diabetes. (22)
One atypical antipsychotic drug, clozapine, is considered unique because it’s the only medication approved by the FDA for treating refractory (recurring) schizophrenia. It is also the only antipsychotic which decreases suicidal thoughts. (23)
Relapses often occur when patients discontinue or take less than their prescribed doses of medication, and these compliance issues are usually related to side effects. Plus, it’s not uncommon for patients to believe their condition has improved and they no longer need the medication they take, although the reason their hallucinations, delusions and negative symptoms of schizophrenia have gone away is because they have been on a drug regimen.
A rare but potentially fatal reaction to antipsychotic drugs is neuroleptic malignant syndrome (NMS). It’s connected to all antipsychotic medications (both first and second generation) and can be identified through symptoms such as “fever, altered mental status, muscle rigidity, and autonomic dysfunction.” Patients who develop these symptoms may die without immediate hospitalization — the mortality rate for NMS is 1 in 10. NMS can occur at any point when taking neuroleptics and happens most often to those on extremely high doses. (24)
Some of the additional, overlapping side effects of these medications include: (25, 26, 27)
- Drowsiness
- Dizziness
- Restlessness
- Weight gain
- High blood sugar
- High cholesterol
- Metabolic syndrome
- Dry mouth
- Constipation
- Nausea
- Vomiting
- Blurred vision
- Low blood pressure (hypotension)
- Uncontrollable movements like tics and tremors (the risk is higher with typical antipsychotics)
- Seizures
- Low white blood cell count
- Sudden cardiac death (due to irregular heartbeat or “arrhythmia”)
Antipsychotic drugs may also be one of the reasons women with schizophrenia have a higher risk of pregnancy and birth complications, although these complications are sometimes due to the disorder itself. (28)
Therapy
While this falls under both conventional and natural treatment of schizophrenia symptoms, therapy is considered an important second-line treatment. I’ll discuss these in more detail later, but one common therapy used in schizophrenia that does not seem to be useful overall is “psychodynamic psychotherapy.” Often used in hospital settings, this talk therapy is based on the concept of building a safe relationship between patient and therapist. A Cochrane review found very little evidence for the validity of this treatment, stating there is “an urgent need for trials” if this is a frequently used intervention. (29)
Electroconvulsive Therapy (ECT)
Sometimes referred to as electroshock therapy, ECT is a medical procedure in which a patient is put under general anesthesia and has electric currents passed through their brain to cause brief seizures. Typically, schizophrenia patients may be given this treatment when experiencing catatonia and where other treatment methods have failed.
ECT has a pretty bad reputation, mostly due to the irresponsible way it was administered in the past (without anesthesia, causing memory loss and physical injury from the seizures). However, it is a much more humane procedure now and may offer some relief when combined with neuroleptic medications.
The Cochrane Review Database reported that electroconvulsive therapy can help to reduce symptoms of schizophrenia more rapidly than medication alone, or for those whose symptoms don’t improve as quickly as the average on antipsychotics. These effects are only known to be of short-term benefit. (30)
How to Help Manage Symptoms
1. Dietary Alterations
Like all conditions, schizophrenia onset is affected, in part, by what a person eats. There is evidence, for instance, that celiac disease may be a precipitating factor for the illness. (16) Having excessive free radical damage and not enough antioxidants circulating is also connected to a higher risk of schizophrenia. (12, 13, 14, 15)
Another dietary risk factor for symptoms of schizophrenia (and their progression) is poor metabolism of essential fatty acids (EFAs). (31) Two fatty acids, arachidonic acid (AA) and DHA, are much lower in patients suffering from schizophrenia and may be increased by some antipsychotics, one possible reason these drugs decrease symptoms. (32)
However, a diet for schizophrenia mirroring what we already know about treating food as medicine will be beneficial for maintaining lower weights and overall health — but it may not help to treat the condition.
For example, a 1999 clinical trial observed participants with schizophrenia eating and supplementing their diet based on food sensitivities and nutrient deficiencies. After five months, patients had improved the blood levels of their nutrients, but no direct symptoms of schizophrenia. (33)
However, that doesn’t mean diet has no impact on this disease. In fact, the ketogenic diet for schizophrenia may be one of the most novel ways to treat symptoms of schizophrenia. The keto diet is a low-carbohydrate, high-fat dietary regimen, first developed in the 1920s for epilepsy. It’s been the subject of both mental illness research and trendy weight loss blogs as of late. Drastically restricting carbohydrates and loading up on fats leads to a bodily process known as ketosis, in which you no longer uses glucose as an energy source and instead rely on ketones from the liver. After the brain transitions from using glucose to ketones and ketosis sets in (between one and seven days), the brain starts using ketones, which affects the way it operates.
There are some impressive case studies (and follow-up animal research) that suggest keto might be a revolutionary natural treatment for schizophrenia. Among the most popular are cases of two women and one man with schizophrenia or schizoaffective disorder who experienced a drastic reduction in all symptoms of schizophrenia while following the diet. (34, 35, 36, 37)
A 2017 review discussed the use of the ketogenic diet in schizophrenia (and other psychiatric disorders). In this review, a small, uncontrolled study in 10 women completed in 1965 (before the dawn of modern antipsychotic drugs) was explained, in which woman on the diet had a “statistically significant decrease in symptomatology” after two weeks. (38)
Now, animal research is being conducted to lead the way into human clinical trials. The first 2015 study found that animals on the ketogenic diet weighed less on average than their placebo counterparts and had less “pathological behaviors” associated with a schizophrenia model in animals. (39, 40)
Why does the ketogenic diet seem to work for schizophrenia? Perhaps it’s because there’s little to no gluten or processed foods on a good ketogenic diet food list, which are known to negatively impact people with risk for schizophrenia? Or maybe it’s the way the keto diet increases antioxidant production and activity? (41) The mechanism is unclear.
A healthy alkaline keto diet consists of foods like:
- Healthy fats (avocado, ghee, MCT oil, coconut oil, olive oil, flaxseed, butter)
- High quality proteins (grass-fed beef, organ meats/offal, turkey, chicken, eggs, tuna, salmon, mackerel)
- Non-starchy veggies (collards, arugula, kale, spinach, broccoli, Brussels sprouts, cauliflower, celery, cucumber, asparagus, tomatoes)
- Bone broth
- Low- or no-carb condiments (spices/herbs, hot sauce, apple cider vinegar, unsweetened mustard)
- Drinks (water, unsweetened coffee/tea, full-fat cow’s/goat’s milk, fresh vegetable juice, sparkling water)
- Full-fat cheeses (in moderation)
- Nuts and seeds
2. Community-Based Recovery Models
Though it may sound impossible to most people, there are low- or no-medication options for recovery from symptoms of schizophrenia that rethink the entire idea behind conventional treatments.
One such method is known as the Soteria paradigm. Founded in the 1970s, Soteria is a community-based recovery model for schizophrenia and related disorders focused on the growth, learning and development for diagnosed patients. Rather than being seen as patients who need to be fixed or controlled, residents at Soteria houses share tasks and responsibilities with staff members. They are given education about their illness and empowered to learn ways to take their future into their own hands.
Reviews of this model have turned out very promising results — residents at Soteria houses have equal or better results than patients treated at traditional psychiatric hospitals and in as little as six weeks. One review remarked that between 85–90 percent of these residents are able to go back to their home and regular routine without taking medication even once! (42, 43) Another reviewer stated that: “Soteria acts like a neuroleptic drug, but without its unfavorable side effects.” (44)
Similar community-based recovery models have been used with results matching those of Soteria. Patients not required to take drugs, and given information about what they were facing reported, as long ago as the 1970s, that their lives were enhanced and the information they received was gratifying and empowering. On the other hand, comparable patients treated in the traditional model expressed frustration and said they were “frozen in the psychosis.” (45)
These results support the Cochrane review about psychoeducation, in which they reviewed available research about what happens when patients are educated about the treatment and symptoms of schizophrenia to find the best possible path to a positive outcome. They concluded: “Psychoeducation does seem to reduce relapse, readmission and encourage medication compliance, as well as reduce the length of hospital stay.” (46)
3. Supplements
A number of dietary supplements have been studied in conjunction with schizophrenia and showed positive results. While a few of these are typically tested for the reduction of medication side effects or other secondary issues, the majority of them help to reduce actual symptoms. An example of supplements for schizophrenia include:
- Omega-3s (47, 48, 50)
- Vitamin D (51, 52)
- L-lysine (53)
- B-complex vitamins (B1, B3, B6, B9, B12) (54, 55)
- Vitamins C and E (56, 57, 58)
- American ginseng (59, 60)
- Sarcosine (also called glycine or N-methylglycine) (61, 62, 63, 64)
- Ginkgo biloba (65, 66, 67, 68)
- Melatonin (to improve sleep quality) (69, 70, 71, 72)
- N-acetylcysteine (NAC or L-cysteine) (73)
- D-alanine (74)
- Bacopa monnieri (75, 76)
- Choline (77, 78, 79)
4. Therapy
Like I mentioned, therapy (subsequent to antipsychotic drugs) is used in conventional treatment of schizophrenia. However, it’s also a completely natural way to deal with schizophrenia and may be tried as an alternative to medication, under proper supervision.
The various types of therapy that may be effective for schizophrenia include:
Cognitive Behavioral Therapy (CBT): This psychotherapy focuses on revealing and changing thought patterns and reactions that are unhealthy therefore altering outward behavior. However, in a Cochrane review, researchers stated, “Trial-based evidence suggests no clear and convincing advantage for cognitive behavioral therapy over other — and sometime much less sophisticated — therapies for people with schizophrenia.” (80)
EMDR: Eye movement desensitization and reprocessing (EMDR) is a popular psychotherapy used to remove stress and fear associated with traumatic memories. EMDR may be particularly effective for people with schizophrenia with PTSD symptoms. (81)
Music Therapy: In a Cochrane review, researchers found that music therapy (in addition to “standard care”) helped to improve “global state, mental state (including negative and general symptoms), social functioning, and quality of life with schizophrenia or schizophrenia-like disorders.” (82)
Animal-Assisted Therapy (AAT): A complementary form of standard therapy, animal-assisted therapy incorporates comforting animals into treatment and may help improve social interactions, general well-being and activities of daily living for individuals with schizophrenia. (83)
Morita Therapy: This case-based therapy is a four-stage, progressive process designed to help individuals accept life “as-is” before trying to make major changes. While all results are preliminary, a Cochrane review did find Morita therapy to be modestly effective in treating schizophrenia. (84)
5. Exercise
Exercising may have beneficial impact on both physical and mental well-being in people with schizophrenia (like it does for us all!). (85) Specifically, yoga has been shown to reduce negative symptoms of schizophrenia as well as improve social skills, although it’s unclear why this happens with yoga in particular. (86)
6. Transcranial Magnetic Stimulation
An alternative, less invasive option to ECT, transcranial magnetic stimulation (TMS) utilizes magnetic fields and stimulates brain nerves. It’s generally used for depression, but a review of randomized, controlled clinical trials found that it’s “effective in reducing [auditory] hallucination rates.” (87)
7. Traditional Chinese Medicine
For over 2,000 years, Traditional Chinese Medicine (TCM) has been used to treat mental health problems, including those resembling schizophrenia. In 2005, a Cochrane review was released that found seven trials observing the impact of TCM on schizophrenia. At that time, the six trials using both TCM and traditional antipsychotics showed the strongest results in improving mental state, overall function and the number of side effects experienced from antipsychotics. Only one small study used only TCM without neuroleptics and did not boast a significant result. (88) Acupuncture is one TCM technique that has already been found to have “antipsychotic effects” in schizophrenic patients. (89)
Precautions
While schizophrenia is not a fatal condition in and of itself, people diagnosed with this disease have lifespans 12–15 years shorter than those without schizophrenia. (90) For that reason, and due to the nature of the condition, it is vitally important for individuals with schizophrenia to be under the care of qualified professionals and to have a solid support system.
Unfortunately, it can be a challenge to find a psychiatrist interested in natural schizophrenia treatments. However, as a family member of, or person with, schizophrenia, it’s important for you to know that there are possibilities that allow a person with schizophrenia to live a very fulfilling life.
That being said, antipsychotics are very strong medications and should not be discontinued or altered in dosage without the supervision of a doctor with experience. Do not stop taking antipsychotic medications without supervision, even if you feel your symptoms have improved and you no longer need it. Always follow recommended dosages on supplements or medications you may take.
Final Thoughts
- Schizophrenia is a mental illness experienced by about 1 percent of the world population (with a slightly higher occurrence in the U.S.). (91) While it is often seen as a completely debilitating disorder, there is a lot of hope for natural ways to manage schizophrenia.
- Typically, individuals are diagnosed with schizophrenia during early adulthood. However, it may be diagnosed (rarely) in children or middle-aged adults. Men present with full psychosis a little earlier than women, but this mental illness affects both genders equally.
- Doctors diagnose schizophrenia by three basic types of symptoms: positive, negative and cognitive.
- Conventional treatment of schizophrenia focuses on first-line drug treatment with antipsychotics/neuroleptics. Therapy and electroconvulsive therapy (ECT) are also used secondarily to these drugs.
- Many patients with this disorder have issues with compliance, meaning they don’t keep taking prescriptions they are given due to a combination of factors.
Note: Do not discontinue your prescriptions without supervision by a qualified medical professional.
Read Next: Borderline Personality Disorder: 4 Natural Ways to Help BPD Treatment












