This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Stopping Superbugs in 4 Steps
June 5, 2016

Have you heard of superbugs? No, they’re not a new horror movie franchise — they’re even more frightening. Superbugs are bacteria that have become resistant to antibiotics, and when treated with the medicines, instead of being wiped out and stopping superbugs, they multiply and thrive.
And these superbugs aren’t just a nuisance — they’re on the cusp of becoming a full-blown public health problem. A recent report warns that if superbugs aren’t stopped in their tracks now, the repercussions are high. These nasty bacteria will be linked to the deaths of 10 million people a year by 2050. That’s one person every three seconds.
What’s the Story Behind Superbugs?
Superbugs were born out of the ashes of the bacteria antibiotics killed. Survival of the fittest? They’ve got it down pat. Superbugs have evolved to be resistant to the very medicines that were created to kill them and even other versions. Some bacteria, for instance, are not only resistant to penicillin, but also to several variations of the antibiotic. (1)
In the U.S., drug-resistant superbugs infect more than 2 million people and kill at least 23,000 each year. (2) Tuberculosis, gonorrhea and pneumonia are all some of the types of diseases that can now survive antibiotic treatment.
While it might seem that antibiotics have been around forever, they’re fairly recent as far as scientific developments go. It wasn’t until 1928 that Alexander Fleming accidentally discovered penicillin. As the “magic” of antibiotics was recognized, diseases that were once a definite death sentence, like malaria and polio, were now treatable.
But as antibiotics became ubiquitous, they started being prescribed for conditions that can be treated via other methods because they work quickly. Then people began taking them for ailments that, by definition, antibiotics can’t help — you won’t recover from the common cold any quicker, for instance, with antibiotics, because antibiotics are useless against viral infections. (3)
How Superbugs Came to Be
Overprescribing antibiotics, combined with skipping doses, sharing antibiotics, not taking medicines at regular intervals as indicated and “saving some for later” are all leading to antibiotic resistance, as superbugs are created.
When someone is treated (or overtreated, as is often the case) with antibiotics, good bacteria are eliminated along with the bad. While sometimes antibiotics are necessary to eliminate diseases, if too much of the healthy bacteria that your body needs are wiped out by them, bad bacteria are able to survive, reproduce and, eventually, become immune to the very drugs meant to eradicate them.
In 2014, the World Health Organization released its first report on antibiotic resistance. It revealed that “this serious threat is no longer a prediction for the future, it is happening right now in every region of the world and has the potential to affect anyone, of any age, in any country.” (4)
As a result, the U.K. established the Review on Antimicrobial Resistance (AMR). The independent body was set up to analyze the problem and propose solutions to combat antimicrobial resistance on a global scale. The results were grim. The AMR study, released in May 2016, found that without a plan that incorporates international cooperation, the world would be “cast back into the dark ages of medicine.” (5)
The report highlighted the supply and demand problem that currently exists globally. The supply of new medicines is not enough to keep up with the increase in drug resistance, as older medicines that had been taken off the market are now being used more widely and microbes have evolved to resist them.
At the same time, the study maintains, the demand for the medicines is very badly managed, with large amounts of antibiotics wasted globally on patients and animals who do not need them, which limits availability for those who can be truly helped by them.
The Superbug Threat
Right on the heels of the report’s release, a woman in the U.S. was found to be infected with bacteria that’s resistant to colistin. (6) This is significant because colistin is an antibiotic that was first released in 1959 but, in the 1980s, was abandoned because it was found to be toxic to the kidneys. (7)
Once antibiotic-resistant superbugs arrived on the scene, colistin and other drugs that were once deemed too dangerous were pulled off the shelves and used as last-resort drugs to treat patients who are immune to other drugs. Now, it seems that the superbugs have found a way to flourish even when being treated with these harsh antibiotics.
The incident likely isn’t isolated. On May 26, 2016, the U.S. Department of Health and Human Services revealed that colistin-resistant bacteria had been found in an American pig. (8) As we know, we are what the animals we eat, well, eat. And while I don’t advocate eating pork, the truth of the matter is that much of the livestock raised in the U.S. is overtreated with antibiotics.
It’s certainly scary to think that if we become seriously ill, the very treatments that should be helping us can be doing more harm than good. Luckily, it’s not all doom and gloom.
The AMR report makes some excellent suggestions for stopping superbugs and reducing antibiotic resistance. It specifically calls out that there needs to be a concerted, international effort to reduce our over-reliance on antibiotics:
Fundamental change is required in the way that antibiotics are consumed and prescribed, to preserve the usefulness of existing products for longer and to reduce the urgency of discovering new ones.
Governments should be held accountable on this goal to reduce the demand for antimicrobials and in particular antibiotics, as should the main sectors that drive antibiotic consumption: healthcare systems, the pharmaceutical industry and the farming and food production industry.
In plain terms, that means the doctors overprescribing these antibiotics, the pharmaceutical companies pushing for sales and the food industries that pump their animals with unnecessary drugs need to be held responsible for their actions.
But as someone looking out for your family, is there anything you can do to help loosen the grip of antibiotics and reduce the risk of superbugs taking hold? Absolutely, you can take steps toward stopping superbugs from becoming an even greater epidemic.
Stopping Superbugs
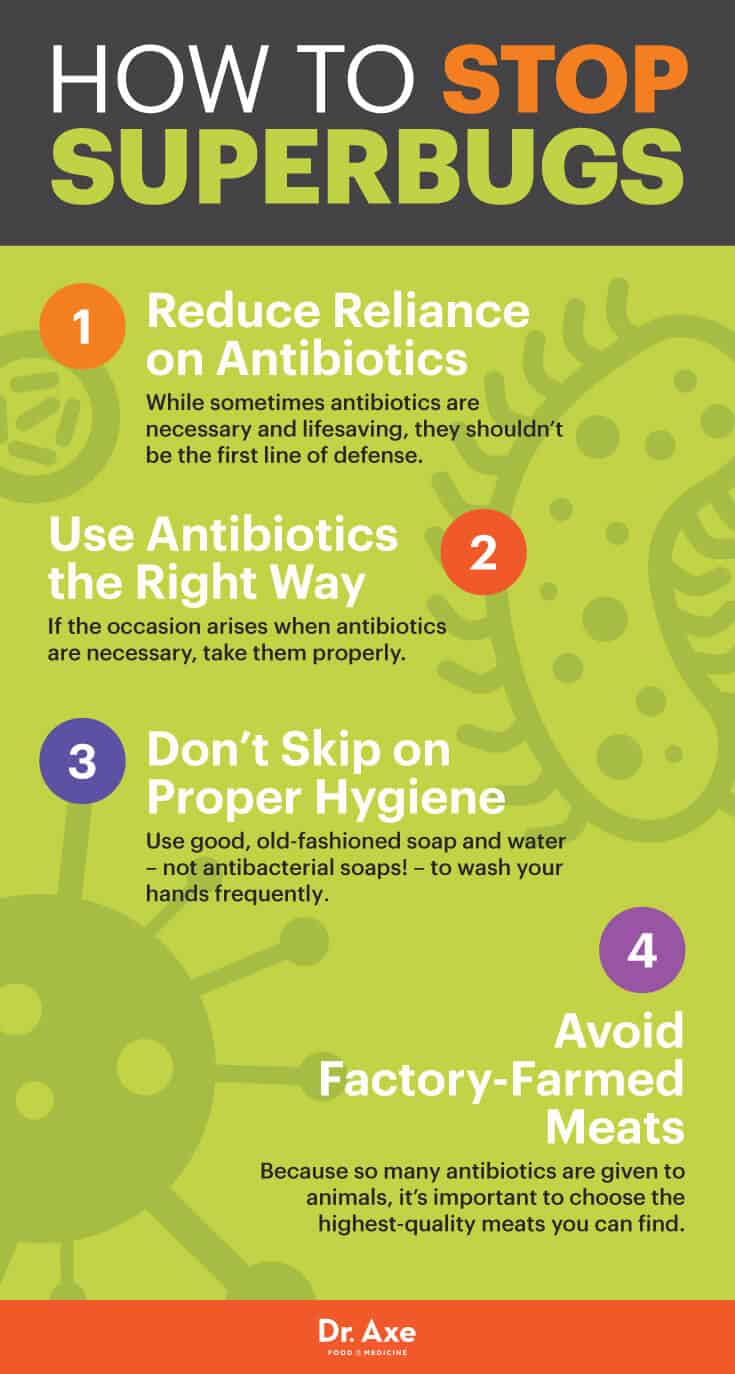
Here are four keys for stopping superbugs:
1. Reduce Reliance on Antibiotics
While sometimes antibiotics are necessary and lifesaving, they shouldn’t be the first line of defense. They should be used as a last-resort option. Unless essential, I encourage you to explore the many natural, non-toxic ways to treat different ailments and conditions, from natural remedies to essential oils.
2. Use Antibiotics the Right Way
If the occasion arises when antibiotics are necessary, take them properly. Take the full, prescribed course as directed. Don’t save medication for later or share with other people.
3. Don’t Skip Out on Proper Hygiene
Use good, old-fashioned soap and water — not antibacterial soaps! — to wash your hands frequently. Avoid close contact with people who are sick to reduce your risk of getting a bacterial infection. If you’re the sick person, think of those around you. Stay home from school or work, and allow yourself to recover so you don’t put others at risk.
4. Avoid Factory-Farmed Meats
Because so many antibiotics are given to animals, it’s important to choose the highest-quality meats you can find. Opt for organic when possible and speak to local butchers at your farmer’s market to find out how the livestock is raised and how they’re treated when ill. What the animals you eat have in their bodies is critical – after all, it will be in yours next.
Expect to see a lot more in the news about superbugs in the coming years. While measures also need to be taken at the government level, we can all do our part in keeping our families a little safer and stopping superbugs from multiplying.